Imagine trying to read a book, recognize a friend’s face, or drive to the store - and suddenly, the center of your vision goes blurry or dark. It’s not a foggy window. It’s your macula failing. This is what happens in age-related macular degeneration (AMD), the leading cause of vision loss for Americans over 65. Unlike cataracts, where the whole lens clouds, AMD quietly eats away at the center of your sight. Peripheral vision stays sharp, but the details vanish - the words on the page, the smile on your grandchild’s face, the lines on the road ahead.
What Exactly Is AMD?
AMD isn’t one disease. It’s two. Most people - about 9 out of 10 - get the dry form. It starts with tiny yellow deposits called drusen building up under the retina. These aren’t harmful by themselves, but over time, they cause the retinal cells to thin out and die. This slow, silent breakdown is called geographic atrophy. You might not notice it at first. Colors seem duller. Reading takes longer. Then, one day, you realize the center of your vision is gone. The other 10-15% develop wet AMD. This is the dangerous one. Abnormal blood vessels grow from the choroid - the layer beneath the retina - and leak fluid and blood right into the macula. These vessels are fragile. They bleed. They swell. And they destroy photoreceptor cells in weeks, not years. That’s why wet AMD causes rapid, severe vision loss. Even if you started with dry AMD, it can turn wet at any time. There’s no warning. No pain. Just a sudden blur.Why Does This Happen?
Age is the biggest risk factor. If you’re over 75, your chance of having AMD jumps to 35%. But it’s not just getting older. Genetics play a huge role. If a parent or sibling has AMD, your risk triples or even quadruples. Smoking? That’s the worst thing you can do. Current smokers are nearly four times more likely to develop AMD than non-smokers. It’s not just about lung health - smoke damages the tiny blood vessels feeding your retina. Race matters too. White people are 2.5 times more likely to get AMD than African Americans. Why? It’s tied to differences in how the retina handles oxidative stress and inflammation. High blood pressure and cholesterol also raise your risk. So does obesity. A BMI over 30 more than doubles your chances. It’s not just about your eyes - it’s about your whole body. At the cellular level, AMD is a slow burn. The retinal pigment epithelium (RPE), the layer that feeds and cleans up the photoreceptors, gets overwhelmed. It can’t remove waste. Lipofuscin builds up. Immune cells attack. The complement system - meant to protect - starts damaging healthy tissue. It’s like your body’s cleanup crew quits, and then the security system turns on the wrong lights.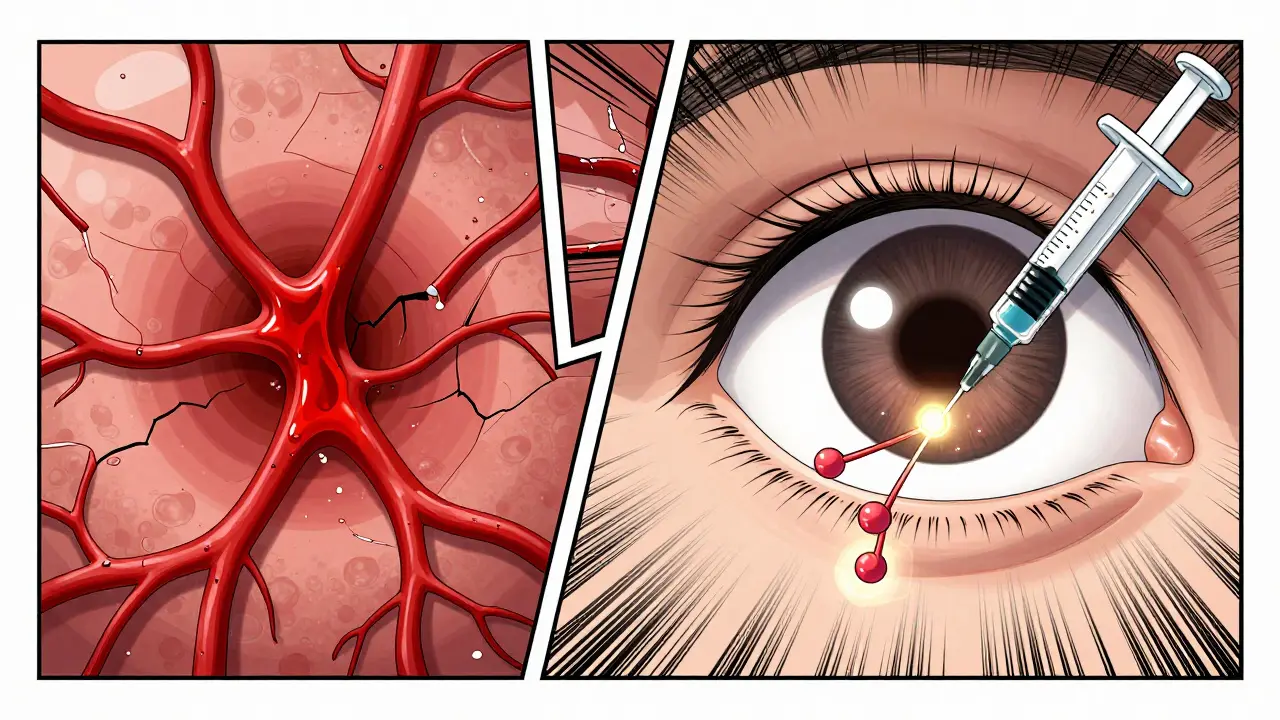
Anti-VEGF: The Game-Changer for Wet AMD
For wet AMD, there’s a powerful tool: anti-VEGF therapy. VEGF stands for vascular endothelial growth factor. It’s a protein your body makes to grow new blood vessels - useful for healing wounds, but deadly in the eye. In wet AMD, too much VEGF triggers those leaky, destructive vessels. Anti-VEGF drugs block it. They don’t cure AMD. But they stop the bleeding. These drugs are injected directly into the eye. It sounds scary, but it’s quick. Numbing drops take the sting away. Most patients say it’s less painful than a dental filling. The first round usually involves monthly shots for three months. Then, doctors watch closely. Using optical coherence tomography (OCT), they scan the retina like a 3D ultrasound. If fluid returns, you get another shot. If it’s stable? You might go 6-8 weeks between treatments. The results? Life-changing. A 2022 survey found 68% of patients on anti-VEGF therapy saw their vision stabilize or even improve. One Reddit user, after 12 injections over nine months, went from 20/200 vision to 20/40. That’s the difference between not recognizing a face and reading a menu.The Burden of Treatment
But there’s a cost. Literally and emotionally. Each injection costs hundreds of dollars. Insurance covers most, but copays add up. And the visits? Patients report 82% find frequent clinic trips exhausting. Missing even one injection can mean losing vision. Studies show people who skip more than 25% of their scheduled shots lose 30% more vision than those who stick to the plan. That’s why new options are coming. In 2021, the FDA approved Susvimo - a tiny implant that delivers ranibizumab continuously for up to six months. No monthly shots. Just a refill every half-year. And in 2022, Vabysmo hit the market - the first drug that blocks both VEGF and another protein called angiopoietin-2. It may mean fewer injections and better long-term results.
What About Dry AMD?
There’s no injection for dry AMD. But there is hope. The AREDS2 study proved a specific vitamin formula cuts progression risk by 25% in people with intermediate AMD. That formula includes vitamin C, vitamin E, zinc, copper, lutein, and zeaxanthin. It doesn’t reverse damage. But it slows it. And if you’re still smoking? Quitting is the single most effective thing you can do. Home monitoring helps too. The Amsler grid - a simple square with a dot in the center and straight lines - is free. Look at it daily. If lines look wavy or the center is blurry, call your eye doctor. Four in ten patients spot wet AMD changes this way before their next appointment.What’s Next?
Researchers are now testing gene therapies that target the inherited complement genes linked to 50-70% of AMD cases. Early trials show promise. Imagine a one-time treatment that resets your body’s faulty immune response. And AI is helping too - algorithms now scan retinal scans to predict who’s likely to progress from dry to wet AMD before symptoms appear. For now, the message is clear: AMD is not inevitable. You can reduce your risk. You can slow it down. And if wet AMD strikes, anti-VEGF therapy can save your central vision. It’s not perfect. It’s not easy. But it works.Can AMD be cured?
No, AMD cannot be cured. Once retinal cells are damaged, they don’t regenerate. But treatments can stop or slow progression. For wet AMD, anti-VEGF injections often preserve or even improve vision. For dry AMD, nutritional supplements like AREDS2 can delay advancement to the more serious stages.
How often do you need anti-VEGF injections?
Initially, patients usually get monthly injections for three months. After that, treatment shifts to "as needed" - meaning injections are given only when fluid reappears in the retina, confirmed by OCT scans. Many patients eventually go 6-8 weeks between shots. Newer treatments like the Susvimo implant can extend this to six months.
Does anti-VEGF therapy work for dry AMD?
No. Anti-VEGF drugs only target abnormal blood vessel growth, which doesn’t occur in dry AMD. Dry AMD is managed differently - through lifestyle changes, AREDS2 supplements, and regular monitoring. Researchers are testing new drugs for geographic atrophy, but none are widely approved yet.
Can you go blind from AMD?
AMD doesn’t cause total blindness. It destroys central vision, so you can’t see details directly ahead - but peripheral vision remains. You can still navigate a room, see movement, and recognize large shapes. That’s why many people with AMD still live independently, especially with low-vision aids and training.
Is AMD only a problem for older people?
While AMD is most common after age 55, it can start earlier. People in their 40s and 50s with strong genetic risks or who smoke can develop early signs. The risk increases sharply after 65, with over one-third of people over 75 affected. That’s why regular eye exams after 65 are critical.