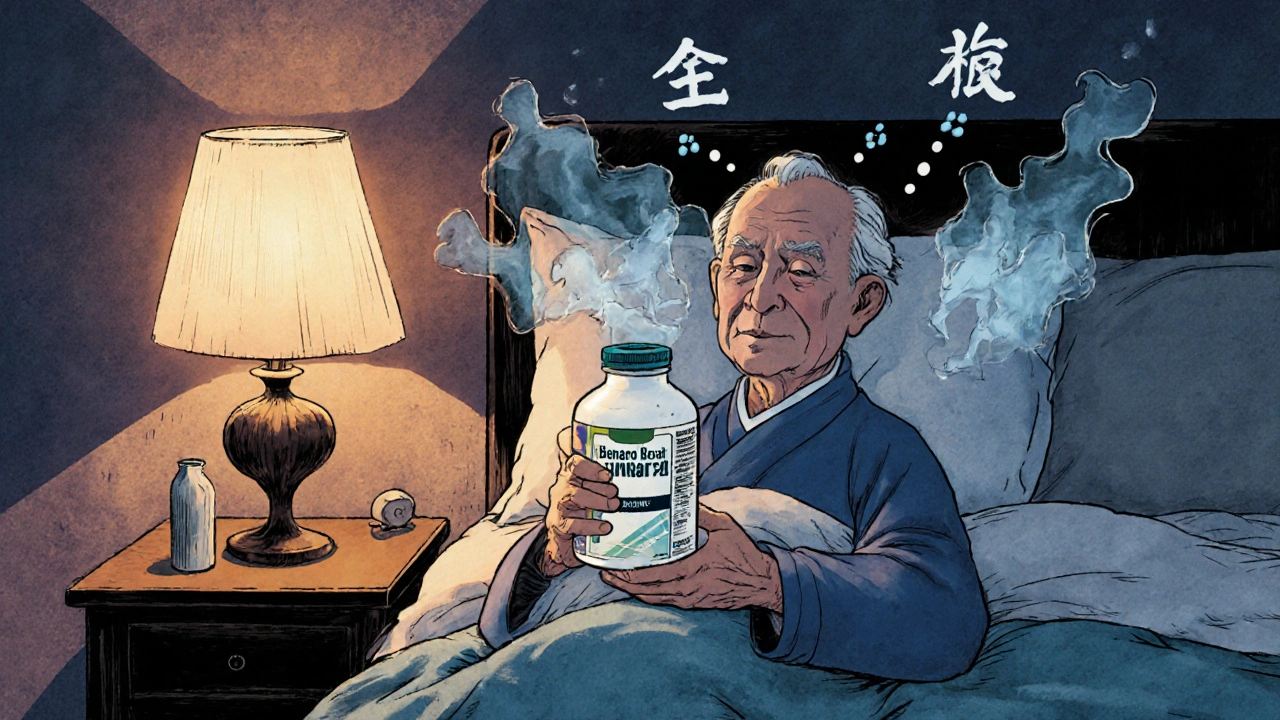
Many older adults reach for over-the-counter antihistamines like Benadryl to help with allergies, colds, or sleep. It’s cheap, easy to find, and works quickly. But what happens when you take it night after night, year after year? A growing body of research suggests that long-term use of certain antihistamines might be linked to higher dementia risk - not because they cause dementia directly, but because of how they affect the brain.
Not All Antihistamines Are the Same
There are two main types of antihistamines: first-generation and second-generation. The difference isn’t just about brand names - it’s about what they do inside your brain.First-generation antihistamines like diphenhydramine (Benadryl), doxylamine (Unisom), and chlorpheniramine cross the blood-brain barrier easily. Once there, they block acetylcholine, a key chemical your brain uses for memory, focus, and learning. This is called anticholinergic activity. That’s why these drugs make you drowsy - they’re slowing down brain activity.
Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) were designed differently. They don’t cross into the brain as easily. Thanks to special transporters that push them back out, their anticholinergic effect is 100 to 1,000 times weaker. They relieve allergies without the foggy feeling.
The American Geriatrics Society’s 2023 Beers Criteria, a trusted guide for safe prescribing in older adults, says first-generation antihistamines should be avoided entirely in people over 65. That’s a Level A recommendation - the strongest possible warning. Yet, millions still take them daily.
What the Studies Actually Show
The biggest fear comes from a 2015 study in JAMA Internal Medicine that followed over 3,400 people aged 65+ for 10 years. It found that people who took strong anticholinergic drugs - including some antihistamines - had a higher chance of developing dementia. But here’s the catch: when researchers looked at antihistamines alone, the link disappeared.A follow-up study in 2019 looked at different drug classes. Antidepressants, bladder medications, and Parkinson’s drugs showed clear increases in dementia risk. But antihistamines? No significant rise. The hazard ratio was exactly 1.00 - meaning no increased risk.
Another study in 2022 tracked nearly 9,000 older adults. It found 3.8% of those using first-gen antihistamines developed dementia, compared to 1% of those using second-gen. At first glance, that looks scary. But after adjusting for age, health conditions, and other medications, the difference wasn’t statistically significant. The numbers were too close to call it a true effect.
Even more confusing? A 2021 meta-analysis that grouped all anticholinergic drugs together claimed a 46% higher dementia risk. But when you break it down, that number was mostly driven by antidepressants and bladder meds - not allergy pills.
The European Medicines Agency says the evidence on antihistamines is inconsistent. The FDA hasn’t added dementia warnings to OTC labels, even though they did for prescription anticholinergics in 2021. Meanwhile, the UK Biobank study published in October 2023 found no link between antihistamine use and dementia once they accounted for underlying sleep disorders - suggesting that people who take these drugs for sleep might already be at higher risk due to poor sleep quality, not the drug itself.

Why the Confusion? It’s Not Just About the Drug
One big problem in this research is that people who take first-gen antihistamines long-term often have other health issues. They’re more likely to have chronic allergies, insomnia, anxiety, or urinary problems - all conditions linked to higher dementia risk. It’s hard to tell if the drug is the cause, or if it’s just a sign of other underlying problems.Also, most studies rely on prescription records or self-reported use. Many people take diphenhydramine for sleep without telling their doctor. They buy it off the shelf. That makes tracking true exposure tricky.
And then there’s the Anticholinergic Cognitive Burden Scale (ACB). This tool rates drugs based on how strongly they block acetylcholine. Diphenhydramine scores a 3 - the highest. Fexofenadine? A 0. That’s why experts say: if you need an antihistamine, choose the ones with a score of 0 or 1.
Real People, Real Concerns
Behind the numbers are real stories. On Reddit, a geriatric care manager wrote that 83% of her clients over 70 take Benadryl every night to sleep. Most don’t know it’s an anticholinergic. On AgingCare.com, a daughter wrote: “My mother’s doctor prescribed Benadryl for years. Now she has dementia. I can’t help but wonder.”These aren’t just fears. They’re valid concerns. Even if science hasn’t proven a direct link, the pattern is troubling enough that experts recommend caution. Why take a risk when safer options exist?

What Should You Do?
If you or someone you care for is taking diphenhydramine or doxylamine regularly - especially for sleep - here’s what to consider:- Switch to second-generation antihistamines. Loratadine, cetirizine, and fexofenadine work just as well for allergies and don’t affect the brain the same way.
- Don’t use antihistamines for sleep. They’re not designed for long-term use as sleep aids. They disrupt natural sleep cycles and can cause next-day grogginess, falls, and confusion.
- Ask about CBT-I. Cognitive Behavioral Therapy for Insomnia is the gold standard for chronic sleep problems in older adults. Studies show it works in 70-80% of cases. The downside? Therapists are hard to find, and insurance doesn’t always cover it. But it’s safer than any pill.
- Review all meds every six months. Many older adults take 5+ medications. A pharmacist or doctor can check for hidden anticholinergic burden using the ACB scale.
- Look for alternatives to OTC sleep aids. Melatonin, magnesium, or low-dose doxepin (Silenor) are better options with minimal anticholinergic effects.
The Choosing Wisely campaign, led by the American Board of Internal Medicine, specifically advises against using diphenhydramine for chronic insomnia in older adults. That’s not a suggestion - it’s a clear clinical guideline.
The Bigger Picture
Sales of first-generation antihistamines have dropped 24% since 2015. Second-generation ones have surged. Why? Because awareness is growing. Pharmacies now stock more Claritin and Zyrtec than Benadryl. Drug labels are changing. The FDA is reviewing all anticholinergic medications - with results expected in 2024.The American Geriatrics Society’s 2024 Beers Criteria update, due in June, is expected to tighten these recommendations even further. We’re moving away from blanket warnings and toward drug-specific guidance. That’s progress.
But change takes time. Millions still sleep with Benadryl. Many don’t know the risks. And for those who do, finding a safe, effective alternative can be hard.
The truth? If you’re using a first-generation antihistamine long-term, you’re not alone - but you might be taking a risk you don’t need to. The science isn’t 100% settled, but the safest choice is clear: switch to a second-generation option. Your brain will thank you.
serge jane
November 21, 2025 AT 12:40It's funny how we treat our brains like they're disposable batteries you swap out when they start to dim. We pop a Benadryl because sleep is elusive, not because we're lazy but because the world doesn't stop for rest anymore. And then we act shocked when memory slips in later years. The brain isn't some machine you can fog up with anticholinergics and expect to run clean for decades. It's a living network, delicate, adaptive, and easily thrown off balance by things we think are harmless. The science may be messy but the pattern is clear: long-term chemical crutches create long-term cognitive debt. We don't need more studies to tell us that. We need more humility.
And yet here we are, still reaching for the blue bottle like it's a lullaby in a pill. We've outsourced sleep to pharmacy shelves while ignoring the root causes - stress, light pollution, poor routines, emotional exhaustion. Maybe the real dementia risk isn't the drug, it's the culture that lets us believe quick fixes are enough.
Switching to Zyrtec is easy. Changing how we live? That's the real challenge.
Nick Naylor
November 21, 2025 AT 23:36Let’s be unequivocally clear: the so-called ‘link’ between antihistamines and dementia is a statistical artifact, a confounder-rich, methodologically flawed narrative peddled by overzealous geriatricians with a bias against OTC medications. The JAMA study? Underpowered for antihistamine-specific analysis. The 2022 cohort? Adjusted for comorbidities that are causally linked to both insomnia AND dementia - not the drug! The ACB scale? A heuristic, not a biological law. The FDA hasn’t issued a warning - because there’s no credible evidence! This isn’t science; it’s fearmongering dressed up as public health guidance. Second-gen antihistamines are not ‘safer’ - they’re just less sedating. That’s it. Don’t let bureaucrats dictate your sleep hygiene based on correlational noise.
rob lafata
November 23, 2025 AT 12:12Oh please. You’re telling me that a generation of grandmas popping Benadryl like candy for 20 years isn’t contributing to the dementia epidemic? You’re the guy who thinks ‘correlation isn’t causation’ until it’s your mom’s brain fogging up. Let me break it down for you: if a drug blocks acetylcholine - the same neurotransmitter that’s depleted in Alzheimer’s - and you take it nightly for a decade, you’re not ‘just sleeping,’ you’re performing a slow, chemical lobotomy on your own hippocampus. And now you want to debate study design? That’s like arguing whether smoking causes lung cancer because ‘some smokers live to 90.’
Here’s the real problem: you’re not the one whose father forgot your name. I am. And I’m tired of people treating dementia like a theoretical puzzle instead of a family tragedy.
Switch to Claritin. Or don’t. But don’t pretend your ignorance is wisdom.
Matthew McCraney
November 25, 2025 AT 10:56They’ve been hiding this for decades. Big Pharma doesn’t want you to know that your $5 Benadryl is part of a covert neurotoxin campaign. The FDA approved it in the 50s knowing the acetylcholine link. They even had the studies. But why warn people when you can sell millions of pills to seniors who can’t remember why they walked into the kitchen? And now they’re pushing Zyrtec like it’s magic? Nah. Same company. Same lab. Just rebranded. They’re testing a new version that’s even more addictive - just less drowsy so you’ll keep buying it. I’ve seen the documents. The whistleblower was silenced. Sleep is a natural process. Pills are control. Wake up. The government doesn’t care. But I do. Share this before it’s deleted.
Brianna Groleau
November 26, 2025 AT 03:29I just want to say - I’m 68 and I used to take Benadryl every night for years. I didn’t know what anticholinergic meant. I just knew I needed to sleep. When my daughter found out, she didn’t yell. She didn’t guilt-trip me. She just sat down with me, opened her laptop, and showed me the difference between Benadryl and Zyrtec. She said, ‘Mom, you’ve been fighting sleep with a sledgehammer. What if we tried a feather?’
I switched. I started reading before bed. I turned off screens. I drank chamomile tea. I didn’t magically sleep better overnight. But I stopped waking up feeling like I’d been drugged. And my memory? It’s clearer. Not perfect. But better.
I’m not saying everyone has to do this. But if you’re reading this and you’re scared - you’re not alone. And change doesn’t have to be dramatic. Just kind. Just gentle. Just one pill at a time.
Rusty Thomas
November 26, 2025 AT 21:48Okay but like… why are we even debating this? I took Benadryl for years and I’m fine. My grandma took it for 40 years and she’s still knitting sweaters at 92. Meanwhile my cousin took ‘safe’ Zyrtec and still got dementia. So what’s the real villain here? Maybe it’s just aging? Or maybe we’re all just scared of getting old and we need a villain to blame? I’m not saying don’t switch. I’m saying stop turning every OTC pill into a dystopian thriller. Also - can we talk about how weird it is that we’re all suddenly experts on neurochemistry? I didn’t even know what acetylcholine was until this post. And now I’m terrified of my allergy meds? 😅
Sarah Swiatek
November 28, 2025 AT 11:55Let’s be real - the real tragedy here isn’t the drug. It’s that we’ve turned sleep into a problem to be fixed, not a rhythm to be restored. We’ve got grandmas taking Benadryl because they’re lonely, because their kids are busy, because their pain isn’t being managed, because their lives have shrunk to a bedroom and a TV. The anticholinergic burden? That’s the symptom. The loneliness, the isolation, the lack of care? That’s the disease.
And yes, switching to Claritin is smart. But if you’re going to do that, why not also call your parent? Why not help them get CBT-I? Why not sit with them in silence instead of handing them a pill? The science tells us one thing. The humanity tells us another. We’re so busy analyzing the mechanism that we’ve forgotten to ask: why did they need it in the first place?
Also - yes, the data is messy. But so are we. And messy people deserve better than convenience.
Dave Wooldridge
November 28, 2025 AT 21:20They’re using this ‘dementia risk’ thing to push you toward Big Pharma’s new expensive sleep drugs. You think Zyrtec is safe? It’s just the gateway. Next they’ll say melatonin is toxic. Then magnesium. Then sunlight. They’re building a world where you can’t sleep without a prescription, a subscription, and a 300-page consent form. I’ve seen the patents. They’re already testing a new class of ‘cognitive-enhancing’ sleep aids that reverse the anticholinergic effect - but only if you pay $200 a month. Don’t be fooled. This isn’t health. It’s control.
Rebecca Cosenza
November 29, 2025 AT 19:24Switch. Now. 😌
swatantra kumar
November 30, 2025 AT 22:22Bro, I’m from India and here everyone uses antihistamines like candy - no doctor, no prescription. We call it ‘sone ka dawa’ - medicine for sleep. But guess what? Our dementia rates are way lower than the US. Why? Maybe because we eat turmeric, walk 10k steps a day, and don’t sit in front of screens till 2am? Maybe the problem isn’t the pill - it’s the whole lifestyle? Just saying. Also, I switched to cetirizine and now I sleep like a baby. 🌙✨
Cinkoon Marketing
December 1, 2025 AT 21:52Actually, I work in pharma marketing and I can tell you - the whole ‘dementia risk’ narrative was amplified by a nonprofit grant-funded initiative that got a little too excited about their own data. The real push behind second-gen antihistamines? Market saturation. Benadryl’s patent expired in the 90s. Zyrtec? Still under patent. The ‘warning’? More of a sales tactic than a scientific revelation. Don’t get me wrong - I’m not saying Benadryl is perfect. But the fear? Manufactured. The science? Still evolving. The marketing? Very, very real.