Baseline CK Test Decision Guide
Is Baseline CK Testing Needed?
This tool helps determine if a baseline creatine kinase (CK) test is clinically indicated for patients starting statin therapy based on current guidelines and evidence.
When you start a statin, your doctor might order a blood test for creatine kinase (CK). But do you really need it? For most people, the answer is no. But for some, skipping this test could mean missing a red flag-or wrongly blaming the statin for symptoms that have nothing to do with it.
Why CK Testing Matters at All
Creatine kinase (CK) is an enzyme found in muscle tissue. When muscles get damaged-whether from intense exercise, trauma, or a drug reaction-CK leaks into the bloodstream. High levels can signal muscle injury. With statins, that’s the main concern: statin-induced myopathy, which ranges from mild muscle aches to rare but deadly rhabdomyolysis. The problem? Muscle pain is common. About 5-10% of people on statins report it. But fewer than 0.1% develop serious muscle damage. Most of those aches aren’t caused by the statin. That’s why blindly blaming the drug leads to unnecessary stops-about 15-20% of patients who quit statins because of muscle pain could have safely stayed on them, if they’d had a baseline CK test to compare against.When Baseline CK Testing Actually Helps
The real value of a baseline CK test isn’t in preventing problems. It’s in interpreting them later. Think of it like taking your blood pressure before starting a new medication. If you feel dizzy weeks later, you need to know if your pressure was already low-or if the drug caused the drop. Same with CK. People vary wildly in their normal levels. One person might have a CK of 120 U/L and never have issues. Another might run at 350 U/L because they lift weights or have a genetic quirk. If you don’t know their baseline, a CK of 280 might look normal to the lab-but to them, it’s a 130-point spike. That’s meaningful. Baseline testing is most useful when:- You have pre-existing muscle or nerve conditions like ALS, muscular dystrophy, or chronic back pain with weakness.
- You have kidney problems (eGFR below 60 mL/min/1.73m²). Reduced kidney function slows statin clearance, raising muscle toxicity risk.
- You’re on high-intensity statins like atorvastatin 40-80 mg or rosuvastatin 20-40 mg. The risk of myopathy jumps from 0.05% to 0.3% annually with these doses.
- You’re taking other drugs that interact with statins-like amiodarone, fibrates, or cyclosporine. These can spike statin levels and muscle damage risk.
- You’ve had statin intolerance before. If you quit a statin due to muscle pain in the past, you’re more likely to react again.
- You’re over 75 or have hypothyroidism. Both increase susceptibility to muscle side effects.
What the Guidelines Say (And Why They Disagree)
Not all medical groups agree on baseline CK testing. That’s because the evidence isn’t black and white. The American College of Cardiology (ACC) and American Heart Association (AHA) don’t require it for everyone. But their 2022 Statin Intolerance Tool says: “Measure CK before starting if risk factors are present.” They’re not saying skip it-they’re saying tailor it. The European Society of Cardiology calls it optional (Class IIb). They argue it adds cost and anxiety without changing outcomes. A 2016 Cochrane Review of nearly 48,000 patients found no difference in myopathy rates between those monitored and those not. But Japan’s guidelines require it for everyone. Why? Because studies show Japanese patients have a 12.7% rate of muscle symptoms versus 7.3% in Western populations. Genetics, diet, and body size may play a role. And the American Association of Clinical Endocrinologists (AACE) says: “Do it for everyone.” Level A evidence, they say. Their logic? Preventing one case of rhabdomyolysis is worth the cost of thousands of baseline tests. The truth? There’s no one-size-fits-all. But there is a smart, targeted approach.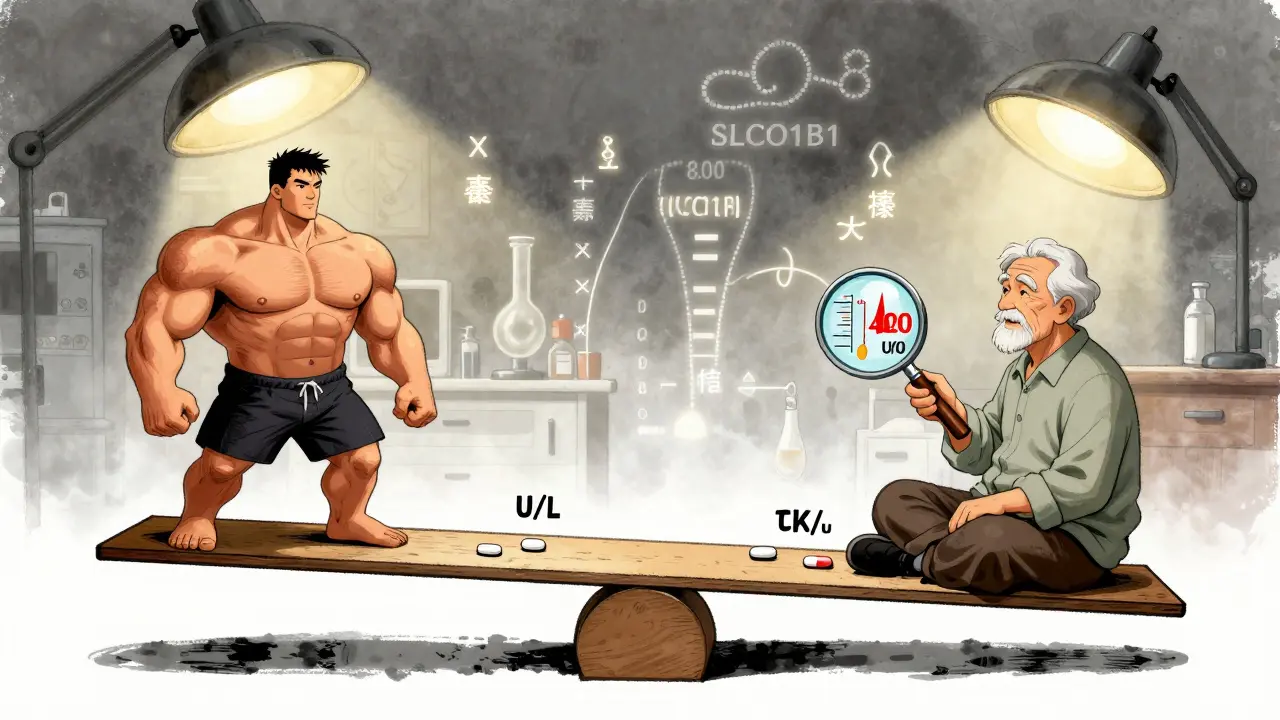
What the Numbers Don’t Tell You
Here’s a surprising fact: 25-30% of healthy people have CK levels above the lab’s “normal” range. Why? Because normal isn’t universal. Men typically have higher CK than women. African Americans often have levels 50-100% higher than Caucasians. Athletes? High. People who recently got a shot in the arm? High. Someone who ran a 5K the day before the test? Very high. That’s why labs report a range-not a single number. And why a baseline test matters so much. If your CK was 400 U/L before you started a statin, and now it’s 450? You’re fine. But if your baseline was 120 and now it’s 450? That’s a red flag. The 2012 STOMP study showed that even asymptomatic people on high-dose atorvastatin had CK levels rise by an average of 20.8 U/L. That’s subclinical-no symptoms, no danger. But without a baseline, you wouldn’t know it was normal for them.When to Test-and When Not To
Do test baseline CK if:- You’re starting a high-intensity statin.
- You have kidney disease, hypothyroidism, or are on interacting drugs.
- You’re over 75.
- You’ve had muscle pain on statins before.
- You’re on a statin-fibrate combo (risk of myopathy is 6-15 times higher).
- You’re starting a low- or moderate-intensity statin (like pravastatin or fluvastatin).
- You’re young, healthy, active, and have no risk factors.
- You’re taking statins for primary prevention (no heart disease yet) and have no symptoms.

What Happens If CK Is High?
If you develop muscle pain and your CK is elevated, here’s how doctors respond:- CK under 3x ULN: No change. Keep the statin. Most symptoms aren’t drug-related.
- CK 3-10x ULN with symptoms: Pause the statin. Check thyroid and kidney function. Re-test CK in a week. Consider switching to a different statin.
- CK over 10x ULN: Stop the statin immediately. This is rhabdomyolysis territory. Hospitalization may be needed.
What’s Coming Next?
New tools are on the horizon. Genetic testing for the SLCO1B1 gene variant can identify people at 4.5 times higher risk of simvastatin myopathy. It’s not routine yet-but in high-risk groups, it could replace CK testing entirely. Point-of-care CK devices are in late-stage trials. Imagine getting your CK result in 15 minutes during your doctor’s visit. No waiting. No confusion. Just clarity. Real-world data from the 2023 Statin Safety Registry shows clinics that do baseline CK testing have 22% fewer unnecessary statin stops. That’s not just good medicine-it’s good economics. Avoiding one unnecessary discontinuation saves about $2,850 per patient, especially in those with heart disease who need statins to stay alive.Bottom Line: Don’t Test Everyone. Test Smart.
Baseline CK testing isn’t about fear. It’s about context. If you’re healthy, young, and on a low-dose statin? Skip it. You’re not at risk, and the test won’t help. But if you’re older, have kidney issues, take other meds, or have a history of muscle pain? Get the test. It’s not about preventing side effects-it’s about knowing when they’re real and when they’re not. Your statin is one of the most proven drugs in medicine. Don’t quit it because of a vague ache. But don’t ignore a real muscle problem either. Baseline CK gives you the data to tell the difference.For the right people, it’s not just useful-it’s essential.

Janette Martens
December 29, 2025 AT 20:05Marie-Pierre Gonzalez
December 30, 2025 AT 13:09Louis Paré
December 30, 2025 AT 18:25Celia McTighe
January 1, 2026 AT 11:14Ryan Touhill
January 2, 2026 AT 19:15Mimi Bos
January 4, 2026 AT 03:29Payton Daily
January 4, 2026 AT 13:56Kelsey Youmans
January 5, 2026 AT 20:04Sydney Lee
January 7, 2026 AT 16:54