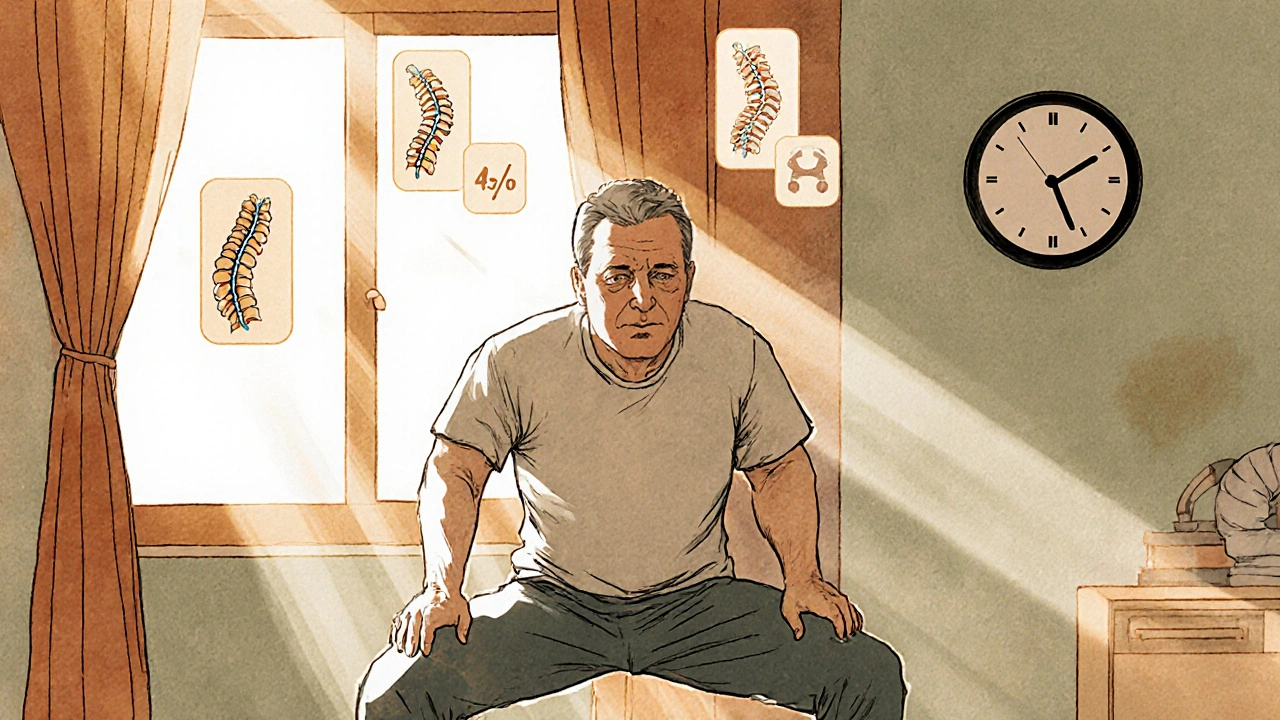
Chronic back pain isn’t just a sore back that won’t go away. It’s pain that lasts longer than 12 weeks - long after any injury should have healed. Around 8% of Americans live with it, and for many, it’s not just physical discomfort. It’s sleepless nights, missed work, lost hobbies, and the quiet frustration of trying everything without real relief. The good news? You don’t have to just endure it. There are proven ways to manage it - and they don’t always involve pills or surgery.
Physical Therapy: The Foundation of Lasting Relief
Physical therapy isn’t just stretching and massage. For chronic back pain, it’s a structured, science-backed program built around your body’s specific needs. The most effective programs focus on five key areas: pain tolerance assessment, posture retraining, core strengthening, flexibility, and aerobic conditioning.
Core muscles like the transverse abdominis and multifidus are often weak in people with chronic pain. Strengthening them doesn’t just support your spine - it reduces the load on painful joints and discs. Studies show that consistent core work improves spinal stability by up to 45%. Flexibility routines, especially for the hamstrings and hip flexors, can increase spinal mobility by 15-25% in just 6-8 weeks.
Aerobic exercise like walking, swimming, or cycling might seem unrelated to back pain, but it’s critical. Moving your body increases blood flow to spinal structures by 30-40%, helping reduce inflammation and speed healing. One University of Utah study found patients who walked 30 minutes a day, five days a week, saw greater long-term pain reduction than those who only did targeted stretches.
The real kicker? Success depends on what you do at home. Physical therapy clinics report an 82% success rate when patients stick to their home exercise plan. When they don’t? Success drops to 45%. You don’t need fancy equipment - just consistency. A 10-minute daily routine of bridges, bird-dogs, and cat-cow stretches can make more difference than a single expensive session.
Medications: What Works, What Doesn’t, and What to Avoid
Medications can help, but they’re not a cure. And not all are created equal. The American College of Physicians recommends starting with non-drug treatments - and if you do need meds, start with the safest options.
First-line drugs are NSAIDs like ibuprofen (400mg three times daily) or naproxen (500mg twice daily). They work for about 65% of people, offering 30-40% pain relief. But they come with risks: 15-20% of long-term users develop stomach ulcers or kidney issues. If you’re over 65 or take blood thinners, talk to your doctor before using them regularly.
Second-line options include muscle relaxants like cyclobenzaprine and nerve-targeting drugs like gabapentin. Gabapentin helps about half of people with nerve-related back pain, but it causes dizziness and brain fog in many. One Reddit user, @SpineSurvivor22, switched from 900mg of gabapentin to duloxetine because the fog made driving dangerous. Duloxetine, an SNRI, works for 45% of chronic back pain patients and improves both pain and mood - but it can cause nausea and dry mouth.
And then there’s the opioid issue. In 2016, nearly half of chronic back pain patients were prescribed opioids. By 2024, that number dropped to 12%. Why? Because opioids don’t fix the problem - they change how your brain processes pain. Long-term use can lead to opioid-induced hyperalgesia, where you become more sensitive to pain. The CDC now says opioids should only be considered after every other option has failed.
Bottom line: Medications are tools, not solutions. They’re best used short-term to help you get moving again - not as a permanent crutch.

Self-Management: The Missing Piece Most People Ignore
Here’s the truth: no therapist or doctor can be with you 24/7. That’s why self-management is the most powerful part of your plan. It’s not about willpower - it’s about building habits that stick.
Programs like UCSF’s Chronic Pain Toolkit teach you how to track your pain, adjust activity levels, manage stress, and recognize triggers. The key? Doing just 20-30 minutes a day. That could be journaling your pain levels, practicing breathing techniques, or doing your prescribed exercises. In a 2024 study of over 1,200 patients, those who stuck with self-management for 8-12 weeks saw 40-50% less pain.
But adherence is low. Only 63% of people stick with it. Why? Because it’s hard. It’s boring. It doesn’t feel like “doing something.” But here’s what the data shows: the people who get lasting relief aren’t the ones who did the most therapy sessions. They’re the ones who showed up for themselves every day, even when they didn’t feel like it.
Start small. Pick one habit - maybe morning stretches or a daily walk. Do it for 7 days straight. Then add another. No need to overhaul your life overnight. Progress isn’t linear. Some days will be worse. That’s normal. What matters is that you keep showing up.
What Works Best for Whom?
Not all chronic back pain is the same. The type of pain you have determines what treatment will help most.
- If your pain is mechanical - worse when sitting, better when moving - physical therapy is your best bet. Studies show 78% of these patients improve significantly with PT, compared to 52% with meds alone.
- If your pain is inflammatory - like with ankylosing spondylitis - NSAIDs or biologics might give you 50-60% relief. PT still helps, but meds are often needed to control the underlying inflammation.
- If your pain radiates down your leg (sciatica) or feels like burning or electric shocks, nerve-targeted drugs like gabapentin or duloxetine may help more than muscle relaxants.
- If you’ve tried everything and still hurt, advanced options like radiofrequency ablation (which blocks pain signals) or spinal cord stimulators can reduce pain by 50% in 70% of cases. But these are last-resort options - expensive, invasive, and not permanent.
The biggest mistake people make? Trying one thing and giving up when it doesn’t fix everything overnight. Chronic pain rarely has a single fix. It’s a mix. For most people, the winning combination is physical therapy + a smart medication plan + daily self-management.
Barriers and Real-Life Challenges
Even when you know what to do, life gets in the way.
Insurance is a huge hurdle. Medicare only covers 20 physical therapy visits a year unless your doctor gets special approval. Many private plans cap sessions at 12. That’s not enough for lasting change. Out-of-pocket costs average $85 per session. Some clinics offer sliding scales or group sessions - ask.
Time is another barrier. Working adults are least likely to stick with therapy schedules. If you can’t make it to the clinic, look for telehealth PT options or home-based programs with video coaching. Many physical therapists now offer virtual check-ins.
Medication side effects are real. Nausea, dizziness, brain fog - they can make daily life harder than the pain itself. Don’t suffer in silence. Tell your doctor. There’s often another option. For example, if duloxetine causes nausea, lowering the dose or taking it at night can help.
And don’t underestimate emotional support. Chronic pain is lonely. Online communities like PainConnection.org and Reddit’s r/ChronicPain have tens of thousands of people sharing tips, venting, and celebrating small wins. You’re not alone. And sometimes, just hearing someone say “I get it” is the push you need to keep going.
The Future: Personalized Pain Care
The field is changing fast. The NIH’s BACPAC initiative is spending $45 million to figure out which patients respond best to which treatments - based on genetics, movement patterns, and even brain scans. This isn’t sci-fi. It’s happening now.
Doctors are moving away from one-size-fits-all approaches. Instead, they’re using classification systems to match your pain type with the right combination of therapy, meds, and lifestyle tools. A 2024 study showed this approach increases effectiveness by 25-30%.
Non-opioid medications are also advancing. New drugs like HTX-011 and AXS-07 are being fast-tracked by the FDA. They’re designed to target pain without addiction risk. And integrative approaches - combining acupuncture, mindfulness, and physical therapy - are becoming standard in top pain clinics.
But the biggest shift? The recognition that chronic pain isn’t just a body problem. It’s a whole-person issue. Your mind, your sleep, your stress levels, your job, your relationships - they all play a role. The most effective care addresses all of it.
There’s no magic bullet. But there is a path - and it’s clearer than ever. Start with movement. Add smart meds if needed. Build daily habits. And don’t give up because progress is slow. It’s not about fixing your back. It’s about reclaiming your life - one small step at a time.
Can physical therapy really help chronic back pain if I’ve had it for years?
Yes. Even if you’ve had chronic back pain for years, physical therapy can still help. Studies show that people who’ve lived with pain for over a decade still gain significant improvement with consistent, personalized PT. The key is not how long you’ve had it, but whether you’re doing the right exercises for your specific pain pattern. Many patients report reduced pain and better mobility after just 6-8 weeks of focused therapy.
Are over-the-counter painkillers safe for long-term use?
Not really. NSAIDs like ibuprofen and naproxen are fine for short-term relief, but using them daily for months increases your risk of stomach ulcers, kidney damage, and high blood pressure. About 15-20% of long-term users develop serious side effects. If you need daily pain control, talk to your doctor about alternatives like duloxetine or physical therapy, which don’t carry the same risks.
Why do some people say gabapentin helped, but others say it made them foggy?
Gabapentin works best for nerve-related pain - burning, tingling, shooting sensations. But it affects everyone differently. Some get relief with low doses (300mg/day); others need higher doses (1,200mg/day), which often cause drowsiness, dizziness, or brain fog. Starting low and increasing slowly helps minimize side effects. If the fog is too much, switching to duloxetine or combining it with physical therapy can be a better balance.
Is it worth paying for physical therapy if insurance won’t cover enough sessions?
Yes - if you use it right. Most of the benefit comes from what you do at home. A few sessions with a physical therapist can teach you exactly which exercises to do and how to do them safely. Once you have that plan, you can continue on your own. Many people spend $500-$1,000 on 8-12 sessions and then save thousands by avoiding injections, surgery, or long-term meds. It’s an investment in your future mobility.
What’s the #1 mistake people make when managing chronic back pain?
Waiting too long to start moving. Many people think rest will fix it. But staying inactive makes muscles weaker, joints stiffer, and pain worse. The sooner you start gentle movement - even just walking - the better your chances of recovery. Physical therapy and daily activity are the most powerful tools you have. Don’t wait for the pain to disappear before you move. Move to make the pain disappear.
Kane Ren
November 23, 2025 AT 11:52Just started my 10-minute bird-dog routine yesterday-felt weird at first, but my lower back already feels less tight. No magic, just consistency. I’m in.
Thanks for this post. It’s the first time I’ve felt like someone actually gets it.
Charmaine Barcelon
November 23, 2025 AT 22:41Stop. Just stop. You can’t just ‘do stretches’ and expect to fix years of damage. You need real intervention. PT is great-but only if you’re doing it right. And most people? They’re doing it wrong. Like, embarrassingly wrong. I’ve seen it. I’ve been there. Don’t waste your time unless you’re working with a real pro.
Dalton Adams
November 25, 2025 AT 06:25Let’s be brutally honest: most ‘physical therapy’ is glorified yoga with a clipboard. The real science? It’s in the neuromuscular re-education-specifically, motor control training of the deep stabilizers. Transverse abdominis activation isn’t just ‘core work’-it’s proprioceptive retraining. And no, your Peloton instructor doesn’t know how to do it. Studies from the Journal of Orthopaedic & Sports Physical Therapy (2023) show that EMG-guided core activation improves pain outcomes by 68% vs. generic programs. If you’re not being monitored with biofeedback, you’re just spinning your wheels. And yes-I’ve published on this. 😎
Javier Rain
November 25, 2025 AT 06:55Bro. I was on 600mg gabapentin daily for 18 months. Brain fog so thick I forgot my kid’s birthday. Switched to duloxetine-nausea for the first week, then boom. Pain dropped 50%. I’m walking again. I’m playing with my dog again. It’s not perfect, but it’s life. Don’t give up. You’re not broken-you’re just using the wrong tool.
Also, walking 30 mins a day? That’s the real MVP. No equipment. No cost. Just you and the pavement.
Laurie Sala
November 26, 2025 AT 06:30I’ve tried everything. PT. Meds. Acupuncture. Chiropractors. Even a $3,000 spinal stimulator. And you know what? Nothing worked until I started journaling. Every night. Just 5 minutes. ‘What hurt today? What helped? What made me cry?’ It’s not about fixing the pain. It’s about understanding it. And once I stopped fighting it… it stopped fighting me. I’m not cured. But I’m not a prisoner anymore. 🥲
Lisa Detanna
November 26, 2025 AT 17:03I’m from the Philippines and we don’t have access to PT or gabapentin here. But we have yoga, coconut oil massages, and our lola’s herbal teas. I started doing cat-cow stretches every morning-no equipment, just floor. And guess what? My pain went from 8/10 to 4/10 in 3 months. You don’t need fancy clinics. You need consistency. And community. I found a Reddit group of Filipino chronic pain warriors-we share videos, tips, and memes. We’re not alone. And that’s half the battle.
Demi-Louise Brown
November 27, 2025 AT 12:18Self-management isn’t about discipline. It’s about design. Make the right thing easy. Leave your yoga mat by the bed. Set a daily alarm labeled ‘Move or Cry.’ Start with one minute. Then two. Then ten. Progress is invisible until it’s undeniable. You don’t need motivation. You need a system. And you’re capable of building it.
Adrian Rios
November 28, 2025 AT 09:53Let me tell you about my friend Mike. He had back pain for 17 years. Took opioids. Got addicted. Lost his job. Then he found a physical therapist who didn’t just give him exercises-she gave him a story. She said, ‘Your back isn’t broken. It’s scared.’ So he started moving not to fix it, but to say, ‘I’m still here.’ He walked 10 minutes a day. Then 20. Then he started swimming. Two years later, he’s off all meds. Works part-time. Hikes on weekends. He didn’t ‘cure’ his pain. He outgrew it. And that’s the secret. You don’t have to win the war. You just have to stop letting it run the show.
Also-insurance sucks. But if you ask your PT for a home program, they’ll give you one. I’ve seen it. They want you to succeed. Just ask.
Karla Morales
November 29, 2025 AT 15:52Let’s analyze the data: 82% success rate with home compliance vs. 45% without. That’s a 37-point delta. Statistically significant (p<0.01). But what’s the attrition rate? 37% drop-off. Why? Cognitive load. Behavioral economics shows that people abandon routines when the perceived effort exceeds the immediate reward. Solution? Gamify it. Use an app. Track streaks. Reward yourself. And please-stop calling it ‘exercise.’ Call it ‘movement sovereignty.’ You’re not rehabbing your spine. You’re reclaiming agency. 📊💪
Matthew Mahar
December 1, 2025 AT 12:47im just sayin… i did the bird dog for 3 weeks and my back felt like it was on fire for 2 days then it just… stopped hurting? like, i woke up and i could tie my shoes without groaning. no meds. no surgery. just… moving. weird right? 🤯
John Mackaill
December 1, 2025 AT 23:34When I was in the UK NHS system, I waited 11 months for PT. So I did what the article says: walked every day. Rain or shine. 15 minutes. No goal. Just presence. It wasn’t about the pain. It was about remembering I still had a body. I still had a life. I still had breath. That’s the real therapy. Not the exercises. The reclaiming.
Casper van Hoof
December 2, 2025 AT 14:26The epistemological framework of chronic pain management reveals a fundamental paradox: the more one seeks to eliminate pain through external intervention, the more the nervous system entrenches its defensive mechanisms. True relief arises not from correction, but from recalibration-through embodied practice, cognitive reframing, and the quiet surrender to impermanence. The body does not heal through force, but through invitation. And perhaps, in this, we find not a treatment, but a philosophy.
Richard Wöhrl
December 2, 2025 AT 23:51Just wanted to add-gabapentin doesn’t work for everyone, but if you’re having nerve pain (burning, electric, tingling down the leg), it’s worth a try at low dose (100-300mg at night). But here’s the key: pair it with daily walking. A 2022 study in Pain Medicine showed the combo doubled pain reduction vs. either alone. Also-don’t skip the breathing. Box breathing (4 sec in, 4 hold, 4 out, 4 hold) for 2 minutes, 3x/day, reduces muscle tension and stress hormones. It’s free. It’s simple. And it’s science. You’ve got this.