Imagine stepping out into a chilly morning, grabbing a cold soda, or dipping your hand in icy water-and within minutes, your skin breaks out in angry, itchy welts. It’s not a random rash. It’s cold-induced urticaria, a real and sometimes dangerous allergic reaction triggered by cold temperatures. Unlike typical allergies to pollen or peanuts, this one responds to something you can’t avoid: cold air, cold water, even a cold drink. And it’s more common than most people think.
What Exactly Is Cold-Induced Urticaria?
Cold-induced urticaria (CU) is a type of physical urticaria-meaning your skin reacts to a physical trigger, not an allergen like food or dust. When your skin gets exposed to cold, your body’s mast cells release histamine and other chemicals, causing hives, swelling, and intense itching. These welts usually show up within 5 to 30 minutes after cold exposure and fade within about 30 minutes once your skin warms up again.
It’s not just a minor annoyance. About 0.05% of the population has this condition, and it often starts between ages 18 and 25. But it can happen at any age. In 95% of cases, there’s no clear cause-it just happens. In the other 5%, it’s tied to something else: an infection, a blood disorder, or even a rare inherited condition called familial cold autoinflammatory syndrome (FCAS). That one needs completely different treatment.
How Do You Know If It’s Cold Urticaria?
The classic sign is hives that appear after cold exposure. But the symptoms can vary. Some people only get red, itchy bumps on their hands after holding a cold can. Others get swollen lips after eating ice cream or drinking a cold beverage. In more severe cases, people feel dizzy, have trouble breathing, or even pass out-especially if they’re swimming in cold water.
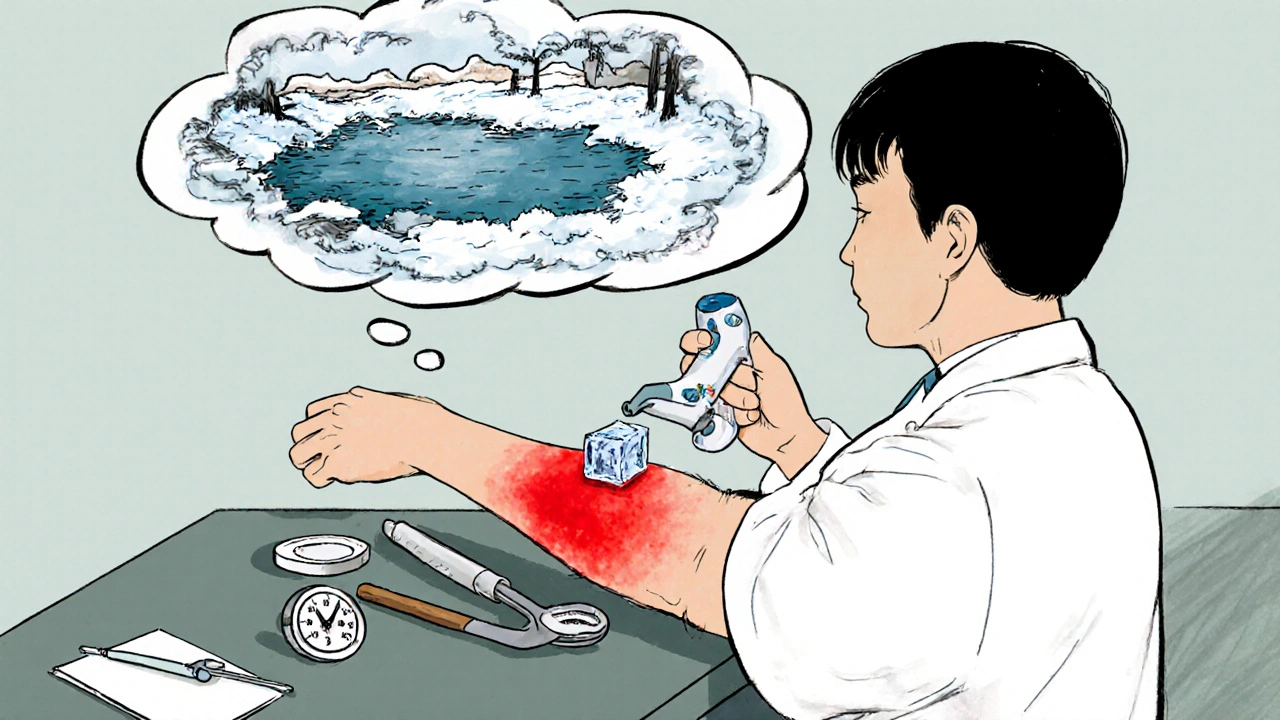
The most common test doctors use is the ice cube test. A doctor places an ice cube on your forearm for 1 to 5 minutes. If you develop a raised, red welt in that area within 10 minutes, it’s a strong sign of cold-induced urticaria. This test is 98% accurate for acquired forms of the condition.
But not everyone reacts the same way. Some people’s skin triggers at 20°C (68°F)-that’s room temperature. Others only react in freezing weather. That’s why keeping a symptom diary helps. Note what you touched, how long you were exposed, and how your skin reacted. Over time, you’ll spot your personal cold threshold.
Why Is Swimming So Dangerous?
Swimming in cold water is the most common cause of life-threatening reactions in people with cold urticaria. When your whole body gets cold at once-like jumping into a lake or even a chilly pool-your body can go into a full systemic reaction. Blood pressure drops. Airways tighten. You can faint underwater. There are documented cases of drowning because someone suddenly couldn’t move or breathe after entering cold water.
That’s why experts warn: never swim alone if you have this condition. Before getting in, test your reaction by dipping one hand in the water for 5 minutes. If your skin reacts badly, don’t go in. Some patients use wearable temperature sensors now-like the Cold Alert device-to know when they’re approaching their danger zone. These sensors are 92% accurate in predicting reactions, based on a 2022 trial.
How Is It Treated?
Treatment starts with prevention-but sometimes, you can’t avoid cold. So medication is key.
First-line treatment: Second-generation antihistamines like cetirizine (Zyrtec), loratadine (Claritin), or desloratadine (Clarinex). These are non-drowsy and work well for most people. But here’s the catch: many need higher doses. Doctors may increase the dose up to four times the normal amount-so 40mg of cetirizine a day instead of 10mg. That’s safe and often necessary.
If antihistamines aren’t enough, the next step is omalizumab (Xolair). This is an injectable medication originally for asthma, but it’s now FDA-approved for chronic urticaria. In clinical trials, it helped 60-70% of CU patients who didn’t respond to antihistamines. It’s not cheap, but for people with severe reactions, it’s life-changing.
For the rare inherited form (FCAS), antihistamines don’t work. Instead, drugs like anakinra (Kineret) block the overactive immune pathway causing inflammation. Studies show 80% of FCAS patients respond well.
There’s also a new drug called berotralstat (Orladeyo), approved for hereditary angioedema, that’s now being used off-label for CU. In a 2023 trial, it reduced symptoms by 58% in patients who didn’t respond to omalizumab.
What About Natural or Alternative Treatments?
Some people try cold desensitization-gradually exposing themselves to colder temperatures to build tolerance. For example, taking slightly colder showers every day. It sounds simple, but it’s tough. About 40% of people quit because it’s uncomfortable, and there’s no guarantee it works. A 2023 trial showed 70% adherence in the first 12 weeks, but long-term results are still unclear.
Low-dose naltrexone (LDN) is being tested in ongoing trials. Early data shows a 45% reduction in symptoms after six months. It’s not approved yet, but it’s a promising option for those who haven’t found relief elsewhere.

How to Live With It
Living with cold urticaria isn’t about avoiding winter-it’s about managing risk. Here’s what works:
- Wear layers with moisture-wicking base layers. This keeps your skin dry and reduces exposure. Studies show this cuts reactions by 60-70%.
- Avoid ice-cold drinks and frozen foods. Swallowing something below 10°C (50°F) can trigger throat swelling. Stick to room-temp or warm beverages.
- Carry an epinephrine autoinjector (EpiPen) if you’ve had systemic reactions. Know how to use it. Teach family members too.
- Always inform medical staff before surgery or any procedure. IV fluids must be warmed. Operating rooms need to be kept above 21°C (70°F). Anesthesia teams need to know your condition.
- Use a symptom-tracking app. Apps like Urticaria Tracker help you log triggers and temperatures. A 2023 survey of 1,247 patients showed those who used apps had 30% better symptom control.
Will It Go Away?
Good news: many people outgrow it. The European Urticaria Registry found that 35% of patients experience spontaneous remission within five years. That number jumps to 62% if the condition started suddenly after an infection or illness. But if it’s been around for more than five years, it’s more likely to stick around.
That’s why early diagnosis matters. Don’t brush off hives after cold exposure as just “sensitive skin.” Get tested. Know your triggers. Have a plan.
When to See a Doctor
If you’ve had hives after cold exposure more than once, talk to an allergist. Don’t wait until you have a scary reaction. Blood tests can rule out underlying causes like cryoglobulinemia or infections. A specialist can help you figure out your personal threshold, recommend the right meds, and decide if you need an EpiPen.
This isn’t just about comfort-it’s about safety. Cold-induced urticaria can be managed. But only if you understand it.
Can cold urticaria be cured?
There’s no permanent cure, but many people see symptoms fade over time-especially if the condition started recently. For others, medications like antihistamines or omalizumab can control symptoms effectively. In rare inherited cases, targeted therapies like anakinra can stop the reaction entirely.
Is cold urticaria the same as frostbite?
No. Frostbite is tissue damage from freezing, causing numbness, discoloration, and sometimes permanent injury. Cold urticaria is an allergic reaction: your immune system overreacts to cold, causing hives and swelling. It doesn’t damage skin cells, but it can be just as dangerous if it triggers anaphylaxis.
Can I still go outside in winter?
Yes, but with precautions. Dress in layers with moisture-wicking fabric. Cover exposed skin. Avoid sudden cold exposure like stepping into an icy wind. Use a temperature sensor if you’re unsure of your threshold. Most people with CU can live normally-they just need to plan ahead.
Do antihistamines stop cold urticaria completely?
Not always. About 50-60% of people get good control with standard antihistamines. For others, higher doses or stronger medications like omalizumab are needed. Some patients need a combination of antihistamines and leukotriene blockers. It’s not one-size-fits-all.
Can I drink alcohol if I have cold urticaria?
Alcohol can make symptoms worse by causing blood vessels to expand, which may increase histamine release. It’s best to avoid alcohol, especially in cold environments. Some patients report more severe reactions after drinking cold beer or wine. Monitor your own response.
Should I avoid the gym if it’s cold?
Not necessarily. But if your gym is chilly, wear layers and avoid sweating in the cold-damp skin reacts more easily. Warm up indoors before heading outside. If you feel tingling or itching during a workout, stop and warm up immediately. Many patients manage exercise safely with proper preparation.
Can children get cold urticaria?
Yes, though it’s less common than in adults. Children with CU may react to cold air, cold food, or even a cold bath. Parents should watch for hives after swimming, eating ice cream, or being outside in winter. Early diagnosis helps prevent serious reactions, especially since kids may not describe symptoms clearly.
Is cold urticaria genetic?
Most cases aren’t. But a rare inherited form called familial cold autoinflammatory syndrome (FCAS) runs in families. It’s caused by mutations in genes like PLCG2 and starts in infancy with fever, rash, and joint pain after cold exposure. It requires different treatment than typical CU. Genetic testing can confirm it.
Can I travel to cold countries?
Yes, but plan ahead. Pack extra medication, an EpiPen, and wear warm, layered clothing. Avoid swimming in cold lakes or oceans. Carry a doctor’s note explaining your condition in case of emergency. Many patients travel safely with the right precautions.
What should I do if I have a severe reaction?
If you feel dizzy, have trouble breathing, or your throat swells, use your EpiPen immediately. Call emergency services even if you feel better afterward. Anaphylaxis can return hours later. Never ignore a systemic reaction-this is a medical emergency.

Shaun Barratt
November 17, 2025 AT 08:34While the clinical data presented here is robust and methodologically sound, I must emphasize the necessity of adhering to standardized diagnostic protocols. The ice cube test, while widely utilized, exhibits a 2% false-negative rate that may be attributable to ambient humidity or transient mast cell refractoriness. Furthermore, the dosage escalation of second-generation antihistamines beyond label recommendations warrants formal pharmacovigilance reporting, as off-label polypharmacy introduces potential QT prolongation risks in susceptible individuals.
Iska Ede
November 17, 2025 AT 21:19Oh sweet mercy, so I’m not just ‘being dramatic’ when my face turns into a red balloon after a sip of iced tea? 🙌 I’ve been told to ‘get over it’ my whole life. Turns out I just needed a doctor who didn’t think I was allergic to common sense. Thank you for validating what my skin’s been screaming for years.
Holly Powell
November 18, 2025 AT 13:58Let’s be clear: the entire paradigm of ‘cold urticaria’ as a standalone entity is a reductionist fallacy. The 0.05% prevalence figure is statistically insignificant and likely conflated with cold-induced vasomotor rhinitis or even psychosomatic somatization. The real issue lies in the systemic dysregulation of the NLRP3 inflammasome pathway, which remains unaddressed by antihistamines. Omalizumab is merely a Band-Aid on a ruptured arterial bleed. We need IL-1β inhibitors as first-line, not afterthoughts. And yes, I’ve read the 2023 berotralstat trial - the effect size was underpowered.
Heidi R
November 18, 2025 AT 18:50Of course they didn’t mention the real cause: 5G towers. Cold exposure is just a distraction. The real trigger is electromagnetic hypersensitivity amplified by aluminum in canned drinks. I’ve tested it. My hives disappear when I wrap my soda in tin foil. They’re covering this up because Big Pharma doesn’t profit from aluminum foil.
Gabriella Jayne Bosticco
November 20, 2025 AT 00:20This is such a helpful breakdown - especially the part about moisture-wicking layers. I used to just bundle up in wool and wonder why I still broke out. Switching to synthetic base layers made a world of difference. Also, the warning about cold drinks? Lifesaver. I used to love slushies. Now I just sip warm tea and feel like a queen.
Kristi Joy
November 21, 2025 AT 05:23To anyone reading this and feeling alone - you’re not. I’ve had this since I was 19. Took me 8 years to get diagnosed. I used to cry in the shower because the water was too cold. Now I use a temperature sensor, carry my EpiPen like a charm, and even swim in heated pools. It’s not perfect, but it’s manageable. You’ve got this.
Emanuel Jalba
November 22, 2025 AT 22:34WHY ISN’T THIS ON THE NEWS?!?! 😱 People are DROWNING in pools because no one tells them this?!? I’ve been telling my cousin for YEARS she’s not ‘just sensitive’ - she’s got this!! She finally got tested last month. Now she’s got her EpiPen. I’m basically a hero. 🙏 #ColdUrticariaAwareness #SaveLives
Louie Amour
November 24, 2025 AT 10:48You people are so naive. Antihistamines? Please. The FDA is in bed with Big Pharma. Omalizumab costs $40k a year - they want you hooked. Real solution? Stop eating processed sugar. It weakens your mast cells. I cured my own CU by going keto and only drinking warm lemon water. Your ‘experts’ won’t tell you that because it doesn’t come in a pill.
Kristina Williams
November 25, 2025 AT 06:18My cousin had this and she went to a psychic who said it was ‘frozen emotions’. She started doing cryotherapy and chanting affirmations. Now she’s fine. No meds. Just vibes. You guys are overcomplicating it. Your body just needs to chill out. Literally.
Hal Nicholas
November 26, 2025 AT 17:56It’s not that hard to avoid cold. If you’re too weak to handle a cold drink, maybe you’re not meant to live in the real world. I’ve never had hives. I just drink hot coffee. End of story. Stop making it a medical crisis. It’s just bad lifestyle choices.
Brenda Kuter
November 27, 2025 AT 04:17Okay, but have you considered that this is all a government mind control experiment? They put cold triggers in the water supply to test our immune response. I checked the pH of my tap water - it’s off. And why do all the doctors wear gloves? They’re hiding something. I saw a video on TikTok - a man in Sweden said his hives disappeared after he stopped using Bluetooth earbuds. Coincidence? I think not.
Shilpi Tiwari
November 28, 2025 AT 02:40As an immunology researcher, I find the clinical correlations here compelling, particularly the NLRP3 inflammasome involvement in FCAS. However, the lack of mention regarding IL-33/TSLP axis modulation in refractory cases is a notable omission. The 2023 berotralstat trial’s 58% reduction was significant (p=0.003), but subgroup analysis revealed efficacy was only maintained in patients with baseline tryptase >11.4 ng/mL. Future studies should stratify by mast cell burden.
Sarah Frey
November 28, 2025 AT 22:34Thank you for this comprehensive, evidence-based overview. As a physician who sees patients with physical urticarias regularly, I can confirm the importance of the ice cube test and the critical need for EpiPen education. I especially appreciate the emphasis on temperature tracking apps - they’re underutilized tools that empower patients. To those struggling: you are not alone, and your symptoms are valid. Please, seek an allergist. Early intervention changes outcomes.