Every year, more than 90% of vision loss from diabetes is preventable-if you catch it early. But here’s the problem: only about 60% of people with diabetes get their recommended eye screening. That’s not because they don’t care. It’s because getting to an eye specialist is hard. Long waits. Dilation drops that blur your vision for hours. Traveling miles for a 20-minute exam. And if you’re in a rural area? Good luck finding anyone who does it at all.
When Should You Get Your First Diabetic Eye Screening?
If you have type 1 diabetes, your first eye exam should happen within five years after your diagnosis. Not sooner. Not later. That’s the rule set by the American Diabetes Association (ADA) 2025 Standards of Care. Why wait five years? Because diabetic retinopathy rarely shows up before then. Screening too early doesn’t help-and it costs time and money.
If you have type 2 diabetes, it’s different. You should get screened right away, at diagnosis. Why? Because many people have had undiagnosed high blood sugar for years before they’re told they have diabetes. By the time they’re diagnosed, early signs of eye damage may already be there. Waiting could mean missing the window to stop it.
How Often Should You Get Screened After That?
Annual screenings are the standard for most people. But it’s not one-size-fits-all. Your doctor will adjust based on what they find.
- If your eyes are completely normal and your HbA1c is under 7%, you might be able to wait every 1-2 years. This is only if you’ve had two or more normal exams in a row and your blood sugar is steady.
- If you have mild diabetic retinopathy, you’ll need to come back in 6 to 12 months.
- With moderate retinopathy, you’ll be seen every 3 to 6 months.
- If you have severe retinopathy or diabetic macular edema (swelling in the center of your vision), you’ll need to be checked every 1-3 months.
- If you’re getting treatment-like laser therapy or eye injections-you’ll need to come in even more often, sometimes every month.
Don’t assume your blood sugar is good enough to skip the exam. A 2023 study showed African American patients develop sight-threatening retinopathy nearly two and a half years earlier than white patients-even with the same HbA1c levels. That’s why personalized screening matters more than ever.
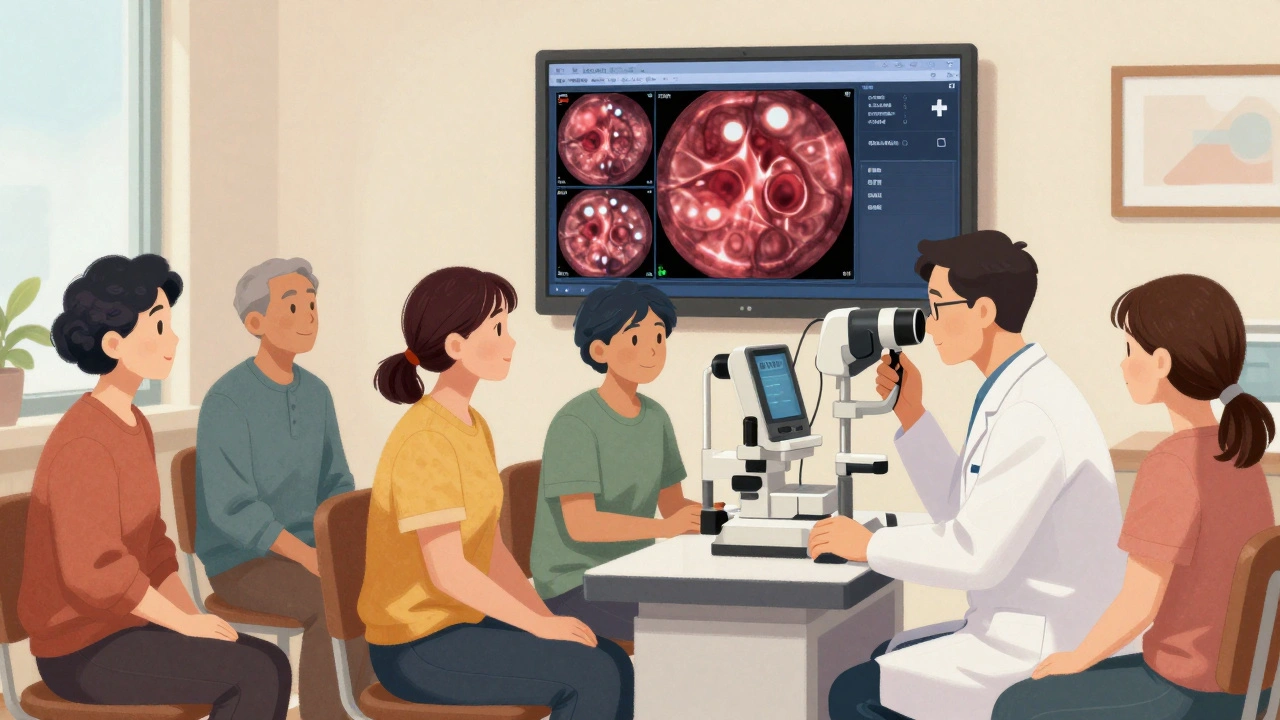
What Happens During a Diabetic Eye Screening?
Traditional screening means dilation. Eye drops widen your pupils so the doctor can see the back of your eye clearly. Then they use a special camera or magnifying lens to look for damaged blood vessels, swelling, or bleeding. It’s effective-but not comfortable. The blurriness lasts 4-6 hours. You can’t drive. You can’t read. You can’t go back to work. Many people skip their exams because of this.
That’s where teleophthalmology comes in.
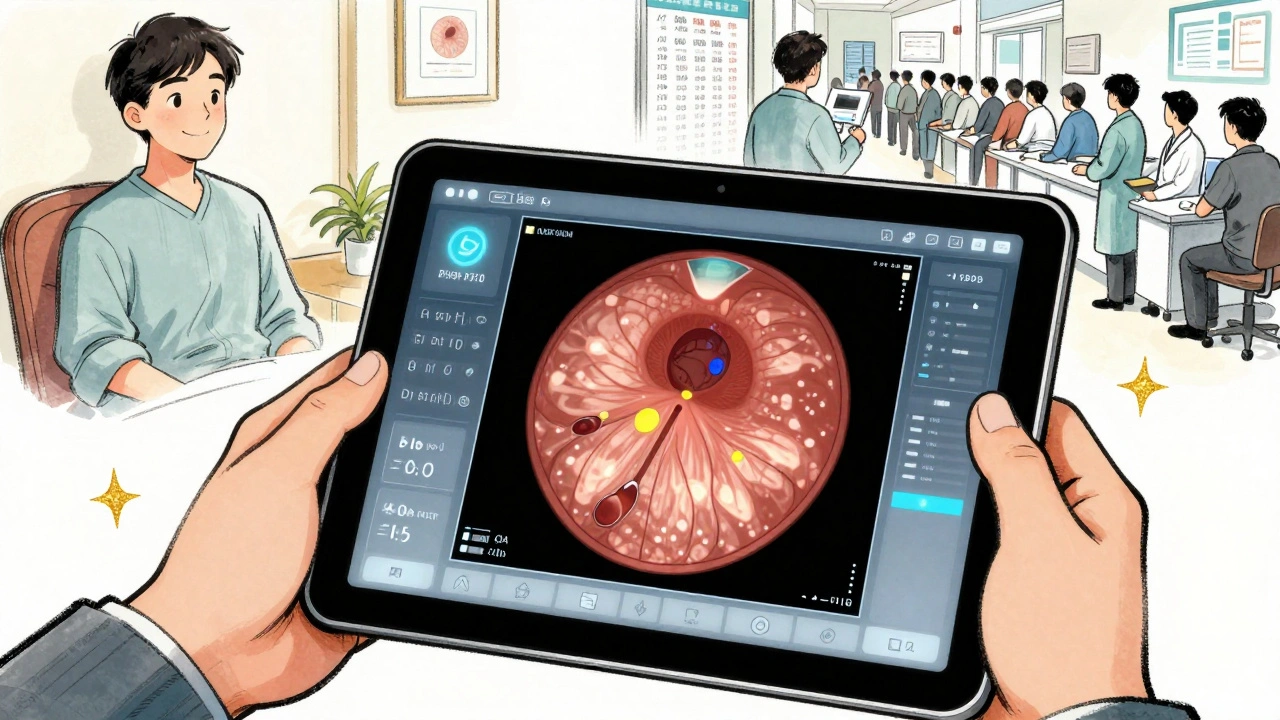
What Is Teleophthalmology and How Does It Work?
Teleophthalmology means getting your eye screening done without stepping into an ophthalmologist’s office. Instead, a non-medical staff member takes digital photos of your retina using a special camera-often right in your primary care clinic or pharmacy. The images are sent securely to a specialist who reads them remotely.
It’s not new. But it’s getting smarter. The FDA approved the first AI system for diabetic eye screening back in 2018: IDx-DR, now called LumineticsCore. It doesn’t need a doctor to interpret the images. The software analyzes them and gives a yes-or-no answer: “More than mild retinopathy detected” or “No referral needed.”
In clinical trials, it caught 87% of cases that needed follow-up and correctly ruled out 91% of healthy eyes. That’s as good as-or better than-many human graders.
Real-world results are even more convincing. In Tamil Nadu, India, a teleophthalmology program screened 15,000 people. Remote experts agreed with in-person doctors 98.5% of the time. In the U.S. Veterans Health Administration, screening rates jumped 32% after they rolled out teleophthalmology across 136 clinics.
Why Isn’t Everyone Using It?
Because it’s not perfect.
First, retinal photos only show the back of the eye. They won’t catch cataracts, glaucoma, or dry eye-common problems in older adults with diabetes. That’s why the ADA still says: if you have symptoms like blurry vision, floaters, or pain, you still need a full eye exam by an ophthalmologist.
Second, setting it up costs money. A single teleophthalmology station can cost $28,500 to install. That’s a big barrier for small clinics, especially in low-income areas. A 2024 study found teleophthalmology adoption was 47% lower in clinics serving Medicaid patients compared to those with private insurance. That’s not progress-it’s a gap widening.
Third, insurance doesn’t always pay for it. In 2024, only 63% of private insurers covered teleophthalmology screenings. Medicare does. Medicaid does in most states. But if you’re on a private plan? You might have to fight for coverage.
How Is Technology Changing the Future?
The next wave isn’t just about taking pictures. It’s about predicting risk.
The T1D Exchange is testing an algorithm that uses 17 factors-not just HbA1c-to predict who’s at highest risk for retinopathy. Things like how long you’ve had diabetes, your blood pressure, cholesterol, kidney function, and even your genetic markers. If you’re low risk, you might only need an exam every three years. If you’re high risk, you’ll be seen more often.
This isn’t science fiction. It’s coming fast. In 2025, the Centers for Medicare & Medicaid Services officially accepted teleophthalmology screenings as meeting the annual screening requirement for quality reporting. That means clinics can now count these exams toward their performance metrics-and avoid payment penalties.
AI-powered screening is already in 22% of Medicare diabetes screenings. In 2022, that number was just 8%. The adoption curve is steep.

What’s Holding People Back?
It’s not just logistics. It’s misinformation.
A 2024 University of Michigan study found 58% of diabetes patients believed keeping blood sugar normal meant they wouldn’t get eye problems. That’s dangerously wrong. Retinopathy can develop even with good control. That’s why screening isn’t optional-it’s essential.
Other barriers? Transportation. A National Federation of the Blind survey found 68% of patients missed exams because they couldn’t get to the clinic. Time. 42% said dilation made them too uncomfortable. And wait times? In big cities, you might wait 37 days just to get an appointment with an eye specialist.
Teleophthalmology solves some of these. You can get screened during your regular diabetes visit. No extra trip. No dilation drops. No blurry vision ruining your day.
What Should You Do Now?
Don’t wait. Don’t assume you’re fine because your blood sugar is good. Don’t skip your screening because it’s inconvenient.
Ask your doctor:
- When was my last eye screening?
- Was it done with a dilated exam or retinal photos?
- Do I qualify for teleophthalmology?
- What’s my risk level for retinopathy?
If your clinic doesn’t offer teleophthalmology, ask why. Push for it. It’s cheaper, faster, and more accessible. And if you’re in a rural area, it might be your only chance to protect your vision.
Diabetes doesn’t just affect your feet and kidneys. It affects your eyes. And your eyes don’t send warning signs until it’s too late. Screenings are your early warning system. Make sure it’s working.
What’s Next?
The future of diabetic eye care is personalized, remote, and AI-driven. But it won’t reach everyone unless we fix the equity gap. Insurance coverage. Clinic funding. Patient education. These aren’t side issues-they’re the core of making sure no one loses their sight because they couldn’t get to a doctor.
If you have diabetes, your eye screening isn’t a luxury. It’s a lifeline. And with teleophthalmology, that lifeline is finally within reach-for more people than ever before.
Iris Carmen
December 8, 2025 AT 14:34so i got my retinal pics done at my doc’s office last month and honestly? no drops, no blurry vision, just sat there like a robot while a machine took pics. felt like sci fi but also… kinda amazing. no more skipping because i can’t drive home.
Raja Herbal
December 9, 2025 AT 23:17in india, we’ve been doing this for years. rural clinics with tablets and cheap cameras. 98% accuracy? sure. but the real win? grandma in village gets screened while buying lentils. no 3-hour bus ride. no ‘sorry we’re booked till june’.
Katherine Rodgers
December 11, 2025 AT 07:21oh wow, AI now reads eyes better than doctors? next they’ll tell me my toaster is diagnosing my diabetes. let me guess - the algorithm is trained on data from people who actually have insurance and don’t live in a trailer park.
Rich Paul
December 13, 2025 AT 05:40you guys are missing the real game-changer: the predictive algorithms. we’re talking multi-parametric risk modeling - HbA1c, BP, eGFR, lipid panels, even SNP markers from GWAS studies. it’s not just screening anymore, it’s stratified intervention. if your risk score is under 0.3, you’re looking at biannual exams. high-risk? monthly monitoring with OCT integration. this isn’t tech - it’s precision medicine 2.0.
Taya Rtichsheva
December 14, 2025 AT 03:28my mom skipped her screening for 3 years cause she said ‘my sugar’s fine’ then woke up one day seeing only shadows… now she’s got laser scars and a new fear of mirrors. why do we only care when it’s too late
Stacy Tolbert
December 15, 2025 AT 07:34i cried reading this. not because i’m dramatic - because i’ve been the person who waited too long. i had mild retinopathy for 18 months before i got screened. i thought ‘it’s just blurry vision, it’ll pass’. it didn’t. if this post saves one person from losing their sight, it’s worth every word.
Lauren Dare
December 15, 2025 AT 13:18so let me get this straight - we’ve got AI that can detect retinopathy better than humans, but we’re still arguing over whether Medicaid should cover it? the system is broken. not the tech. the people running it. someone’s getting paid to keep this inequity alive.
Mona Schmidt
December 16, 2025 AT 09:01thank you for highlighting the disparities in access. teleophthalmology isn’t just a tool - it’s a civil rights issue. if your vision depends on your zip code or insurance type, we’ve failed as a society. we need policy changes, not just tech fixes. clinics serving low-income communities deserve funding, not excuses.
Sarah Gray
December 17, 2025 AT 12:01the fact that you’re still using ‘diabetic eye screening’ as a standalone term reveals your lack of understanding. it’s not ‘diabetic’ - it’s ‘diabetes-related retinopathy screening’. terminology matters. precision matters. if you can’t even get the language right, why should anyone trust your data?
Suzanne Johnston
December 19, 2025 AT 11:44we’ve built machines that see better than our eyes - but we still can’t see the human cost of neglect. the real tragedy isn’t the missed diagnosis. it’s the quiet resignation of people who’ve been told for decades that their health doesn’t matter. technology won’t fix that. only empathy will.
Graham Abbas
December 20, 2025 AT 10:03my cousin in rural Georgia got screened via teleophthalmology last week. she drove 45 minutes to her primary care clinic - not the eye doctor 90 miles away. she got the results in 2 hours. no dilation. no waiting. she cried. not from fear - from relief. this isn’t innovation. it’s justice.
Carina M
December 22, 2025 AT 09:59It is imperative to note that the adoption of AI-driven diagnostic modalities must be preceded by rigorous validation protocols in accordance with ISO 13485 and FDA 21 CFR Part 820. The current regulatory framework does not sufficiently account for algorithmic drift in heterogeneous populations, thereby introducing unacceptable levels of clinical risk.
Ajit Kumar Singh
December 22, 2025 AT 23:55in india we have 1000 people per ophthalmologist and 100000 people per AI camera - so we use both. the camera catches the damage, the doctor catches the truth behind it. one without the other is just noise. this isn’t replacement - it’s partnership. stop treating tech like a magic wand
Simran Chettiar
December 23, 2025 AT 13:22the philosophical underpinning of this entire discourse rests upon the epistemological assumption that medical data, when digitized and algorithmically processed, can transcend the ontological limitations of human perception - yet we remain tethered to the material conditions of healthcare infrastructure, insurance regimes, and socioeconomic stratification, which ultimately determine not merely access, but the very possibility of survival in a system that commodifies vision itself.
Guylaine Lapointe
December 23, 2025 AT 20:05Wow. Just wow. Someone actually wrote something useful for once. I’m shocked. But seriously - if you’re still getting dilated exams in 2025, you’re not being thorough, you’re being stubborn. Get the photos. Save your time. Save your vision. Stop being a martyr to outdated practice.