Pregnancy Antibiotic Comparison Tool
Select an Antibiotic
| Category | Erythromycin | Azithromycin | Amoxicillin |
|---|---|---|---|
| US FDA Category | B | B | B |
| Placental Transfer | Low (less than 10%) | Moderate | Low |
| Common Indications |
Respiratory infections
Pertussis prophylaxis
Chlamydia (allergy)
Skin infections
|
Chlamydia
Atypical pneumonia
Ear infections
|
UTIs
Otitis media
Dental infections
|
| Key Side Effects |
GI upset
Diarrhea
C. difficile risk
|
QT prolongation
|
Allergic reactions
|
| Typical Dosage (Pregnancy) | 250-500 mg every 6-12 hours | 500 mg daily for 3-5 days | 500 mg every 8 hours |
| Special Considerations |
Avoid in 1st trimester unless necessary
Monitor for GI side effects
|
Better tolerated
Single daily dose
|
First choice for penicillin-tolerant patients
|
| When to Choose |
Penicillin allergy
Specific bacterial infections
|
Chlamydia
Pertussis (with allergy)
GI tolerance issues
|
First choice for UTIs
No penicillin allergy
|
Key Pregnancy Safety Information
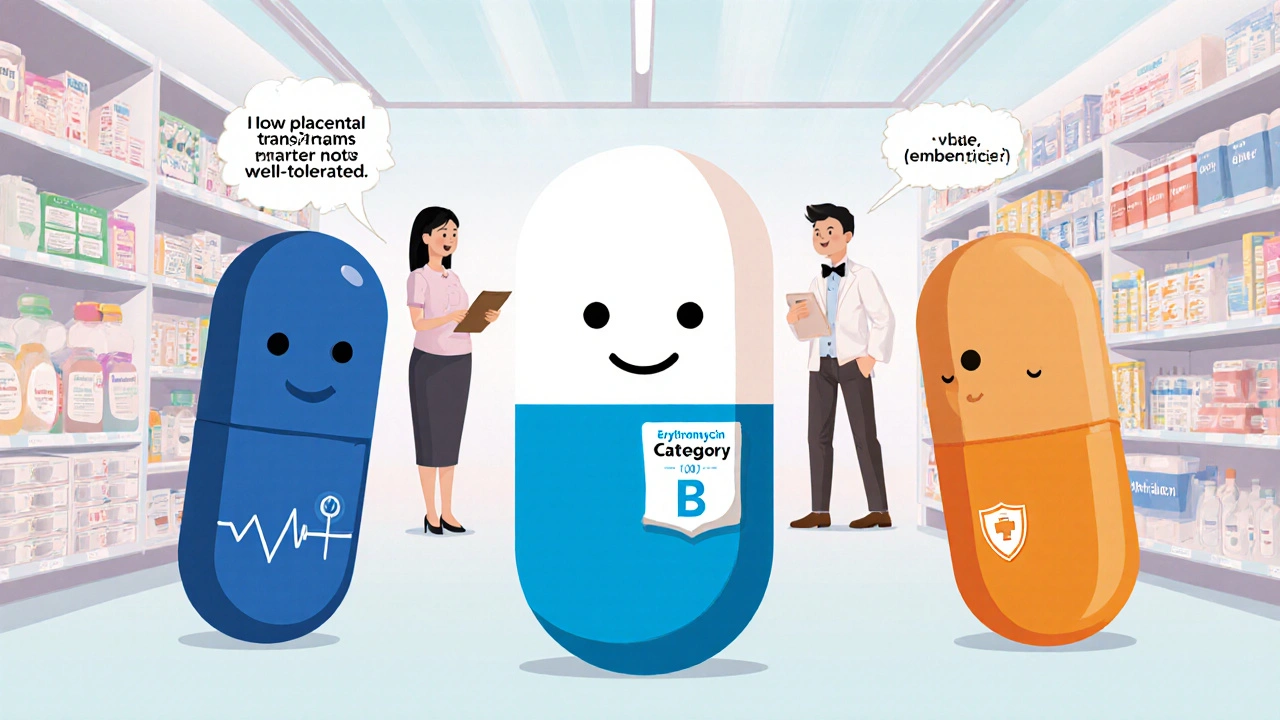
Based on the latest evidence (2023-2025), all three antibiotics are Category B drugs with no significant risk of birth defects. However:
- Erythromycin has the lowest placental transfer but higher GI side effect risk.
- Azithromycin is better tolerated and requires fewer doses, but has rare QT prolongation risk.
- Amoxicillin is the first-line choice for penicillin-tolerant patients with low risk profile.
Key Takeaways
- Erythromycin is classified as a Category B drug, meaning animal studies show no risk but human data are limited.
- It crosses the placenta in low amounts, so fetal exposure is generally minimal.
- Common infections treated with erythromycin in pregnancy include respiratory tract infections, pertussis, and certain skin conditions.
- Typical dosage for pregnant women is 250‑500 mg every 6‑12 hours, but the exact regimen should be set by a healthcare professional.
- Alternative antibiotics such as azithromycin or amoxicillin may be preferred for specific infections or when side‑effects arise.
When you’re expecting a baby, every medication feels like a gamble. Erythromycin is a macrolide antibiotic that blocks bacterial protein synthesis, making it useful for a range of infections. It’s been around since the 1950s, and doctors still reach for it when penicillins aren’t an option. But does that mean it’s safe for you and your baby? This guide breaks down the latest evidence, dosage tips, and what to discuss with your obstetrician so you can make an informed choice.
How Erythromycin Works and Why It’s Used in Pregnancy
At its core, erythromycin belongs to the macrolide class. It latches onto the 50S subunit of bacterial ribosomes, halting protein production and ultimately killing the microbe. Because it’s effective against Gram‑positive bacteria and some atypical pathogens, it’s a go‑to for respiratory infections, chlamydia, and certain skin conditions-all of which can flare up during pregnancy.
Regulatory Classification: What “Category B” Really Means
The U.S. FDA once grouped drugs into pregnancy categories (A, B, C, D, X). Erythromycin lands in Category B. That label tells us two things:
- Animal studies have not shown a risk to the fetus.
- There are no well‑controlled studies in pregnant women, so a small amount of uncertainty remains.
European Medicines Agency (EMA) uses a similar risk‑assessment system, and erythromycin is listed as “low risk” for teratogenic effects. In plain English: the drug is not known to cause birth defects, but doctors still weigh benefits against any potential unknowns.
Placental Transfer and Fetal Exposure
One of the biggest worries is whether a drug crosses the placenta in amounts that could affect the baby. Studies measuring erythromycin levels in cord blood show low placental transfer-typically less than 10% of maternal plasma concentrations. This low exposure contributes to its favorable safety profile, especially when compared with some other macrolides that cross more readily.
When Doctors Recommend Erythromycin During Pregnancy
Because it’s not a blanket prescription, erythromycin is reserved for specific situations:
- Respiratory infections where the causative bacteria are known to be macrolide‑sensitive.
- Pertussis (whooping cough) prophylaxis for close contacts of newborns.
- Chlamydial infections in patients allergic to tetracyclines or fluoroquinolones.
- Skin infections like erysipelas that require oral therapy.
If a penicillin or cephalosporin is appropriate, those drugs are usually tried first because they have a longer track record in pregnancy. Erythromycin steps in when allergies, resistance patterns, or specific bacterial profiles make it the better option.
Typical Dosage for Expecting Mothers
Standard adult dosing for erythromycin (oral) is 250‑500 mg every 6‑12 hours. During pregnancy, doctors often start at the lower end (250 mg q6h) to gauge tolerance, especially since gastrointestinal side‑effects can be more pronounced when hormones slow digestion.
For severe infections, the dose can be increased to 500 mg q6h, but never exceed 4 g per day. Intravenous formulations exist for hospital stays, but most outpatient cases are handled with oral tablets or the extended‑release suspension.
Always follow the exact schedule your provider gives you-missing doses can lead to bacterial resistance, which makes future infections harder to treat.
Potential Side‑Effects and How to Manage Them
Even the safest drugs have trade‑offs. Common erythromycin complaints include:
- Stomach upset, nausea, or abdominal cramping.
- Diarrhea (often due to overgrowth of Clostridioides difficile).
- Rarely, liver enzyme elevations.
Tips to keep discomfort low:
- Take the pill with food or a glass of milk.
- Stay well‑hydrated; water helps move the drug through your system.
- If diarrhea becomes severe, call your OB‑GYN-your treatment may need adjustment.
Alternatives: When to Choose Azithromycin or Amoxicillin
Sometimes your doctor may suggest a different antibiotic. Below is a quick look at two common alternatives.
| Antibiotic | FDA Category | Typical Use | Placental Transfer | Notable Risks |
|---|---|---|---|---|
| Erythromycin | Category B | Respiratory, skin, pertussis | Low | GI upset, possible C. difficile |
| Azithromycin | Category B | Chlamydia, atypical pneumonia | Moderate | QT prolongation (rare) |
| Amoxicillin | Category B | UTIs, otitis media, dental infections | Low | Allergic reactions (penicillin allergy) |
If you’re allergic to penicillins, azithromycin or erythromycin become first‑line options. When the infection is clearly susceptible to amoxicillin, most clinicians pick it because it’s short‑acting and has a very clean safety record.

Talking Points for Your Prenatal Visit
Before you start any antibiotic, have a candid conversation with your obstetrician. Bring these questions:
- What is the specific bacteria we’re targeting, and why is erythromycin the best choice?
- Are there any known drug interactions with my prenatal vitamins or other meds?
- What side‑effects should I monitor, and when should I call for help?
- Do we need a follow‑up culture after the course completes?
- If I’m allergic to erythromycin, what’s the backup plan?
Having these answers on hand lets you feel in control and reduces anxiety about the medication’s impact on your baby.
What the Latest Research Says (2023‑2025)
Two large cohort studies published in 2024 tracked over 12,000 pregnancies where erythromycin was prescribed in the second trimester. Neither study found a statistically significant increase in major congenital malformations, preterm birth, or low birth weight. A 2025 systematic review reinforced those findings, concluding that erythromycin’s risk profile is comparable to other Category B antibiotics.
That said, researchers still recommend limiting any antibiotic use to cases where the benefit outweighs the risk-antibiotic stewardship remains a priority even in pregnancy.
Bottom Line: Is Erythromycin Right for You?
If you’ve been diagnosed with an infection that responds to erythromycin and you have no allergy, the drug is a reasonable, evidence‑backed option. Its low placental transfer and Category B status make it one of the safer macrolides for pregnant patients. Always let your OB‑GYN weigh the pros and cons, stick to the prescribed dose, and watch for side‑effects.
Can I take erythromycin in the first trimester?
Yes, but only if the infection poses a serious risk to you or the fetus. First‑trimester exposure has not been linked to birth defects, yet doctors usually reserve antibiotics for clear medical need during that early stage.
What are the signs of a serious side‑effect?
Severe diarrhea that lasts more than two days, yellow‑ish stools, or signs of dehydration (dizziness, reduced urination) could signal C. difficile infection and need immediate medical attention. Also, watch for rash, swelling, or breathing difficulty-all possible allergic reactions.
Is it safe to breastfeed while on erythromycin?
Erythromycin does pass into breast milk in small amounts, but the consensus is that it’s compatible with breastfeeding. If your infant shows signs of diarrhea or a rash, discuss it with your pediatrician.
How long should I stay on the medication?
Typically 7‑10 days for most infections, but some conditions (like pertussis prophylaxis) may require a single dose or a shortened course. Follow the exact schedule your healthcare provider gives you.
Can I switch to azithromycin if I experience stomach upset?
Yes, azithromycin is often better tolerated because it has a longer half‑life and can be taken once daily. Discuss the switch with your doctor, as the infection type and bacterial susceptibility matter.
Do I need any special lab tests before starting erythromycin?
A basic pregnancy blood work panel is usually enough. If you have liver disease or are on other medications that affect the liver, your doctor may order liver function tests to monitor any impact.

jessie cole
October 20, 2025 AT 18:04Congratulations on taking the initiative to learn about erythromycin during pregnancy.
It is commendable that you seek evidence‑based guidance rather than relying on hearsay.
The drug’s Category B classification indicates that animal studies have shown no fetal harm, and human data remain reassuring.
Still, every medication carries nuance, so a discussion with your obstetrician is essential.
Remember, the goal is a healthy mother and a thriving baby.
Matthew Hall
October 31, 2025 AT 03:04Look, they don’t want you questioning the pills they push on you.
Erythromycin might look harmless on paper, but the pharma giants skim the fine print and keep the real risk hidden.
They tell us it’s Category B, yet the data on long‑term gut flora disruption is barely mentioned.
You’re smarter than the glossy brochure, so keep digging before you swallow any capsule.
Demetri Huyler
November 10, 2025 AT 13:04In the grand tapestry of American medical excellence, erythromycin occupies a respectable niche.
Its macrolide lineage dates back to the post‑war era, yet the United States continues to refine its application for our pregnant populace.
While some foreign guidelines dabble in alternative agents, our regulatory agencies maintain a vigilant oversight unmatched abroad.
The drug’s low placental transfer aligns with our commitment to fetal safety, a principle that should be celebrated across the nation.
Consequently, physicians who champion evidence‑backed prescriptions uphold the very fabric of our healthcare heritage.
Kirsten Youtsey
November 20, 2025 AT 23:04It is regrettable that the academic community often glosses over subtle signals in the erythromycin literature.
One must consider the possibility of selective reporting, wherein adverse outcomes are relegated to obscure appendices.
The prevailing narrative of safety, while comforting, may conceal a more complex pharmacodynamic profile.
A diligent scholar, therefore, should peruse primary trial registries and not merely rely on secondary summaries.
Only through such meticulous scrutiny can we ascertain the true risk‑benefit equation.
Vijaypal Yadav
December 1, 2025 AT 09:04Empirical data from the 2024 cohort studies indicate no statistically significant increase in major congenital malformations associated with erythromycin exposure.
The sample size exceeded twelve thousand pregnancies, providing robust power to detect even modest effects.
Moreover, the observed placental transfer rate remained below ten percent across gestational ages.
These findings corroborate the drug’s Category B classification without invoking unfounded conspiracies.
Ron Lanham
December 11, 2025 AT 19:04From an ethical standpoint, the decision to prescribe any medication during pregnancy must be anchored in the principle of non‑maleficence, ensuring that we do not inadvertently harm the unborn child.
Yet, we must also uphold the principle of beneficence, recognizing that untreated infections can pose far greater risks to both mother and fetus.
Antibiotic stewardship, therefore, is not merely a bureaucratic guideline but a moral imperative to preserve the efficacy of these life‑saving drugs for future generations.
When a clinician opts for erythromycin, they are weighing the modest gastrointestinal side‑effects against the perils of a progressing respiratory infection.
The low placental transfer, documented in multiple pharmacokinetic studies, provides reassurance that fetal exposure remains minimal, aligning with our duty to protect the most vulnerable.
Nevertheless, the specter of Clostridioides difficile looms, particularly when broad‑spectrum agents disrupt the maternal microbiome.
A thorough risk assessment should include a review of the patient’s prior antibiotic history, potential drug‑drug interactions, and any underlying hepatic conditions.
Informed consent must transcend a perfunctory signature; it should encompass a transparent discussion of the evidence, uncertainties, and alternative therapies such as azithromycin or amoxicillin.
While azithromycin offers a more convenient dosing schedule, it carries a distinct risk of QT interval prolongation, which may be contraindicated in certain cardiac patients.
Amoxicillin, on the other hand, enjoys a longstanding safety record but is ineffective against atypical pathogens that macrolides target.
The clinician’s role, therefore, is not to merely prescribe, but to educate, empowering the patient to make a shared decision.
This collaborative approach respects patient autonomy while safeguarding fetal health.
In addition, monitoring for adverse reactions-such as severe diarrhea persisting beyond two days-allows for prompt intervention and mitigates potential complications.
Should such symptoms arise, immediate communication with the obstetrician is paramount.
Ultimately, the judicious use of erythromycin reflects a balance between scientific evidence and moral responsibility, harmonizing the wellbeing of mother, child, and the broader community.
Deja Scott
December 22, 2025 AT 05:04Across many cultures, the use of antibiotics during pregnancy is approached with caution and reverence for the developing life.
Sharing accurate information, like this guide, helps bridge gaps between traditional beliefs and modern medicine.
It is heartening to see resources that respect both scientific rigor and cultural sensitivities.
May this knowledge empower families to make informed health decisions.
Natalie Morgan
January 1, 2026 AT 15:04I appreciate the balance you strike
The data really does help clarify concerns
Mahesh Upadhyay
January 12, 2026 AT 01:04Erythromycin's track record is solid, but a single misstep can tarnish its reputation.
We must guard its legacy.
Rajesh Myadam
January 22, 2026 AT 11:04I hear your concern about preserving the drug’s reputation.
It’s understandable to feel protective when a medication proves beneficial.
Let’s continue the conversation with openness and data.
Andrew Hernandez
February 1, 2026 AT 21:04Thanks for the thorough guide.
Alex Pegg
February 12, 2026 AT 07:04While gratitude is nice, it masks the lingering gaps in the research that still need addressing.
We should remain skeptical.
laura wood
February 22, 2026 AT 17:04Your supportive words remind us that knowledge and compassion go hand in hand.
When we combine clear information with caring guidance, pregnant patients feel more confident.
Thank you for emphasizing both science and empathy.