When your gallbladder stops working right, the pain doesn’t just come and go-it hits like a wave you can’t swim out of. Imagine a sharp, steady ache under your right ribs that lasts for hours, maybe with nausea, fever, or yellowing skin. That’s not just indigestion. That’s your bile system screaming for help. Gallbladder and biliary diseases aren’t rare. About 1 in 6 adults in the U.S. has gallstones, and women are more than twice as likely to get them. Most people never know they have them-until they suddenly do.
What Are Gallstones, and Why Do They Form?
Gallstones are hardened deposits of bile, the fluid your liver makes to digest fat. They form when bile has too much cholesterol, too much bilirubin, or not enough bile salts. About 80% are made of cholesterol. The rest are pigment stones, mostly bilirubin, common in people with liver disease or certain blood disorders. Some stones are tiny like grains of sand; others grow as big as golf balls. They sit quietly in the gallbladder until they move. If one blocks the cystic duct-the tube that drains the gallbladder-you get acute cholecystitis: inflamed, swollen, painful. If it slips into the common bile duct, things get dangerous. That’s when bile backs up, bacteria grow, and you risk cholangitis. Or worse, the stone jams the pancreatic duct, triggering pancreatitis. Risk factors are clear: being female, over 40, overweight, diabetic, or having rapid weight loss. Native Americans, especially Pima Indians, have the highest rates globally-up to 64% in some groups. Asian populations see more pigment stones than Westerners. Obesity triples your risk. So does diabetes.Cholangitis: When the Bile Ducts Get Infected
Cholangitis isn’t just a complication-it’s a medical emergency. It happens when a stone or other blockage traps bile in the ducts, letting bacteria multiply. The classic signs? Charcot’s triad: severe pain in the upper right abdomen, fever, and jaundice. If you add low blood pressure and confusion, you’ve got Reynolds’ pentad-signs you’re heading into septic shock. About 70% of people with cholangitis have abdominal pain. Eighty-five percent have fever. Jaundice shows up in 60-70%. Left untreated, it can kill. That’s why doctors don’t wait. If you have these symptoms, you need imaging and antibiotics fast. ERCP is often the next step-not just to diagnose, but to fix it.ERCP: The Procedure That Saves Lives
Endoscopic Retrograde Cholangiopancreatography (ERCP) is a blend of endoscopy and X-ray. A thin, flexible scope is threaded through your mouth, down your esophagus, past your stomach, and into the duodenum. There, the doctor finds the ampulla of Vater-the opening where bile and pancreatic juices enter the intestine. A tiny catheter is inserted, dye is injected, and X-rays show the ducts in real time. But ERCP isn’t just for pictures. It’s a tool. If a stone is blocking the duct, the doctor can cut the sphincter (sphincterotomy), use a basket or balloon to pull out the stone, or place a stent to keep the duct open. Success rates? Over 90% in experienced hands. Still, it’s not risk-free. About 3-10% of patients develop post-ERCP pancreatitis-the most common complication. It’s worse if you have Sphincter of Oddi dysfunction. Some centers now use preventive stents to reduce this risk. Infection, bleeding, or perforation can happen too. That’s why ERCP should never be used just to look. MRCP, a non-invasive MRI scan, is the first test for suspected bile duct stones. It’s 95% accurate and carries no risk.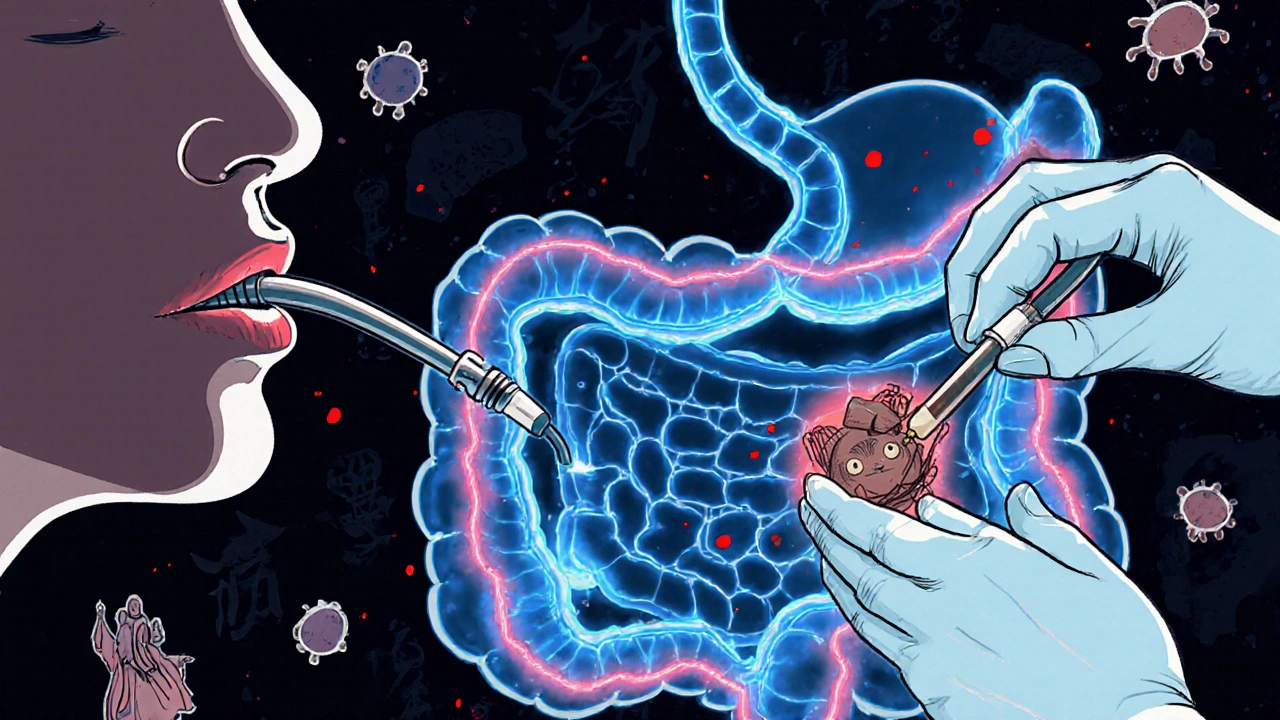
What Happens After Gallbladder Removal?
If you have symptomatic gallstones, the standard treatment is laparoscopic cholecystectomy-removing the gallbladder through small cuts in the abdomen. It’s done in 90% of cases. Recovery is fast: most people go home in a day and back to work in a week. Open surgery? That’s rare now, reserved for complicated cases. Recovery takes weeks. But removing the gallbladder doesn’t mean the story ends. About 12% of people develop post-cholecystectomy syndrome-ongoing pain, bloating, or diarrhea. Why? Without the gallbladder to store bile, it flows constantly into the intestine. Some people can’t handle fatty meals. A low-fat diet for 2-4 weeks helps. Most adapt within 6 weeks. A few need medications like loperamide for diarrhea. And here’s the twist: not everyone needs surgery. If your gallstones aren’t causing symptoms, guidelines say leave them alone. The chance of future problems is only 1-2% per year. Yet, about 20% of the 600,000 cholecystectomies done in the U.S. each year are on people with mild or no symptoms-against current advice.What About Dissolving Stones or Breaking Them Up?
You might hear about pills or shock waves. Ursodeoxycholic acid (UDCA) can dissolve small cholesterol stones under 15mm, but only in 30-40% of cases-and it takes 6 to 12 months. It doesn’t work on pigment stones. And once you stop the pills, stones often come back. Shock wave lithotripsy-breaking stones with sound waves-used to be tried. But recurrence rates hit 50% within five years. It’s rarely used now. The real winners? Prevention and timing. If you’re at risk-overweight, diabetic, losing weight fast-slow it down. Lose no more than 1.5kg per week. Eat regular meals. Don’t skip breakfast. That helps bile flow and reduces stone formation.What’s New in 2025?
Technology keeps improving. In 2023, the FDA approved a new duodenoscope with a fully disposable elevator mechanism. Why? Because old designs were linked to 112 outbreaks of drug-resistant infections between 2013 and 2018. Now, the risky part is thrown away after each use. Intraductal ultrasonography (IDUS) is now used during ERCP to spot tiny stones under 5mm that standard imaging misses. Sensitivity jumps from 75% to 92%. That means fewer missed diagnoses and fewer repeat procedures. Telehealth is helping too. After ERCP or surgery, virtual check-ins have cut 30-day readmissions by 18% in pilot programs. Patients get quicker answers, fewer unnecessary trips to the ER. But a big gap remains. Only 30-40% of patients with bile duct stones get their stones removed during the same ERCP session as their gallbladder surgery. That means extra procedures, extra costs, extra stress. Experts are pushing for better coordination between surgeons and endoscopists to fix this.
What Patients Say
On Healthgrades, 87% of cholecystectomy patients rate their experience 4.5 out of 5 stars. “The pain was unbearable,” one wrote. “After surgery, I felt like a new person.” But Reddit threads tell a different side. “I had ERCP. The recovery was quick, but my throat hurt for five days.” Another: “They didn’t get all the stones. I had to go back-and ended up in the hospital with cholangitis.” And then there’s the diarrhea. “I thought removing my gallbladder would fix everything. Instead, I’m on Imodium every time I eat pizza.” Education matters. Patients who get clear info before ERCP report 78% satisfaction. Those who don’t? Only 52%.When to Seek Help
Don’t wait. If you have:- Severe, constant pain under your right rib for more than 4-6 hours
- Fever with chills
- Yellow skin or eyes
- Nausea and vomiting that won’t stop
Beth Banham
November 8, 2025 AT 17:45Wow, this is such a clear breakdown. I had no idea gallstones were so common. My mom had hers removed last year and she’s been fine since, but I never realized how much goes on behind the scenes with bile and ducts.
Alyssa Salazar
November 10, 2025 AT 02:21Let’s be real-ERCP is the MVP of biliary interventions. Sphincterotomy + stone extraction in one go? Yes please. But seriously, the post-ERCP pancreatitis risk is still terrifying. I’ve seen patients flatline because someone did it ‘just to be safe’ without MRCP first. Stop using ERCP as a diagnostic tool. It’s not a toy. And yes, I’m mad about this. Again.
Jim Oliver
November 11, 2025 AT 11:38Of course 20% of cholecystectomies are unnecessary-because doctors are paid per procedure, not per outcome. Also, ‘low-fat diet for 2-4 weeks’? That’s not a solution, that’s a Band-Aid on a gunshot wound. And why are we still using ‘gallbladder removal fixes everything’ as a marketing slogan? It doesn’t. Ever.
Brierly Davis
November 12, 2025 AT 02:41Y’all are killing me with the ERCP drama 😅 I had mine last year and yeah, my throat was raw for days-but I went from crying in the bathroom to eating tacos in 3 weeks. Life’s better now. Also, the new disposable duodenoscope? Big win. No one wants to be part of an infection outbreak. 🙌
Amber O'Sullivan
November 13, 2025 AT 05:56Why do we even do UDCA anymore it’s a waste of time and money and the stones come back anyway just cut it out already
Rashmi Mohapatra
November 13, 2025 AT 19:17people in india get pigment stones because of poor diet and no protein intake and also too much rice and sugar and they dont even know why their liver is messed up
Lashonda Rene
November 13, 2025 AT 21:24i had gallstones for years and just dealt with it because i was scared of surgery and then one day i woke up and my face was yellow and i ran to the er and they were like oh yeah you need this done now and i was so scared but the whole team was so nice and they did the ercp and then the surgery and now i eat pizza every weekend and no im not on imodium anymore so if you’re scared just go get it checked out youll be fine
Jennifer Bedrosian
November 15, 2025 AT 12:56THEY DIDNT GET ALL THE STONES AND I HAD TO GO BACK AND THEN I GOT CHOLANGITIS AND SPENT 5 DAYS IN THE HOSPITAL AND NOW I CAN’T EAT ANYTHING WITH BUTTER AND MY DOCTOR JUST SMILED AND SAID ‘WELL AT LEAST YOU’RE NOT DEAD’ I HATE MEDICAL SYSTEMS
Ryan Masuga
November 16, 2025 AT 10:07you know what helped me after surgery? walking 10 mins after every meal. no joke. it kept the bile moving and i didn’t get that bloated feeling. also, don’t skip breakfast. my grandma always said that and turns out she was right. slow and steady wins the race, folks.
Andy Slack
November 17, 2025 AT 10:551 in 6 adults? That’s insane. I’m just glad we have MRCP now. No radiation, no cutting, just a scan. Why isn’t this the first step everywhere? We’re still playing medical Russian roulette with ERCP. Fix the system, not just the stones.
William Priest
November 17, 2025 AT 18:56Also, ‘post-cholecystectomy syndrome’? That’s just ‘you didn’t actually have gallstones, you had IBS’. Also, ‘low-fat diet’? That’s not medicine, that’s a diet book. Also, ‘gallbladder removal fixes everything’? No. It doesn’t. Ever. Also, stop doing ERCPs on asymptomatic people. Also, also, also.
Brierly Davis
November 18, 2025 AT 06:58^^^ this. I had mine out and still get bloating sometimes. But I just eat smaller meals and avoid fried stuff. It’s not perfect, but it’s manageable. You’re not broken-you’re just adapting. We all are.