When your kidneys can’t do their job anymore, your body starts to fill up with waste and fluid that should have been removed. Without treatment, this leads to serious illness - even death. That’s where dialysis comes in. Two main types of dialysis are used worldwide: hemodialysis and peritoneal dialysis. Both keep you alive, but they work in completely different ways. Choosing between them isn’t just about medical facts - it’s about your lifestyle, your body, and what you can manage day to day.
How Hemodialysis Works
How Peritoneal Dialysis Works
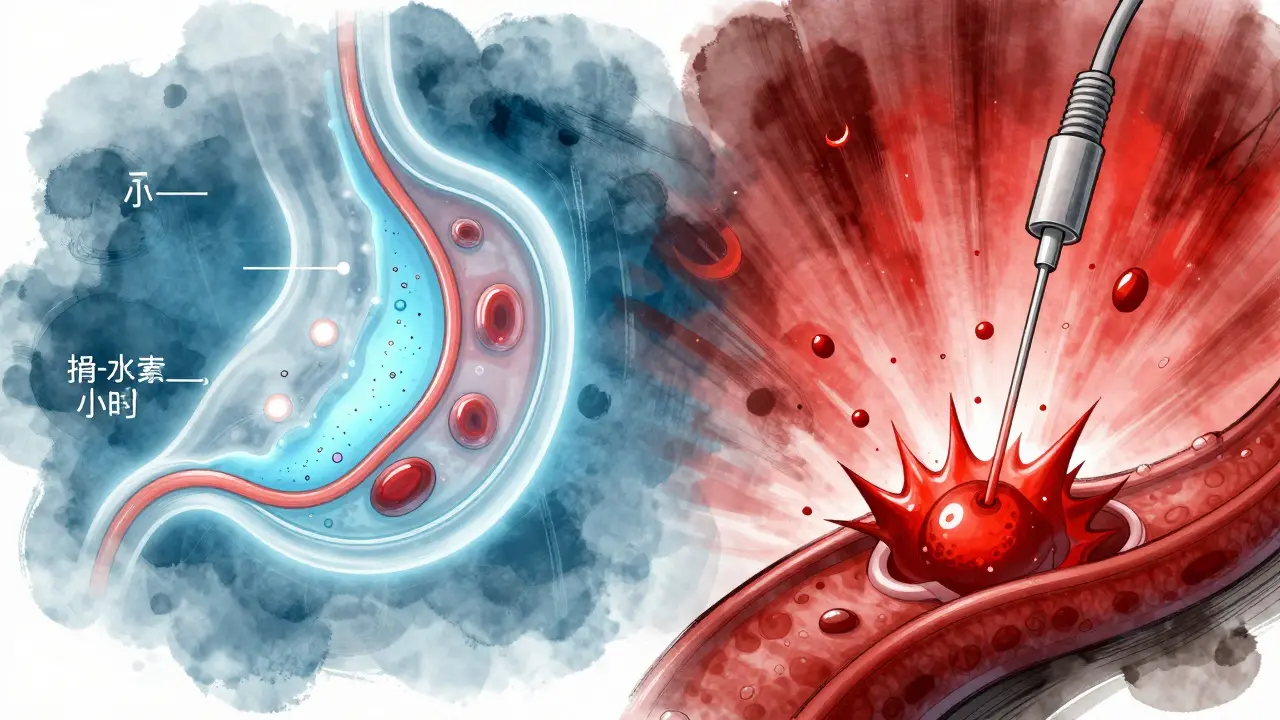
Peritoneal dialysis uses your own belly lining - the peritoneum - as a natural filter. A soft, flexible tube called a Tenckhoff catheter is placed into your abdomen during a short surgical procedure. After about two weeks of healing, you start treatments. You fill your belly with a special fluid called dialysate, usually 1.5 to 3 liters at a time. This fluid sits in your abdomen for 4 to 6 hours, drawing out waste and extra fluid through your peritoneal membrane. Then you drain it out. You repeat this 3 to 5 times a day if you’re doing manual exchanges (called CAPD), or you can use a machine at night while you sleep (called APD).
One big advantage? You don’t need to go to a clinic. Most people do this at home, at work, or even while traveling. No needles. No bulky machines during the day. Just bags of fluid and a catheter that stays in place. But it demands discipline. Every exchange has to be done with clean hands, sterile technique, and careful attention to avoid infection. A single mistake can lead to peritonitis - an infection in the belly that can send you to the hospital.
Key Differences in Procedure and Frequency
Hemodialysis is scheduled. Most people go to a clinic three times a week, for 3 to 5 hours each visit. That’s about 12 hours a week spent hooked up to a machine. The blood is pulled out of your body through a needle in your arm (usually from an AV fistula - a surgically created connection between an artery and vein), cleaned by the dialysis machine, and returned. It’s fast, powerful, and controlled by technicians.
Peritoneal dialysis is continuous. You’re doing small cleans all day or all night. No fixed schedule. You can choose when to do your exchanges. Some people do them during lunch breaks. Others do them all at night while sleeping. The total clearance over a week is similar to hemodialysis - but it’s spread out. This means fewer spikes in toxins and fluid between sessions. You’re less likely to feel sick, bloated, or exhausted after a treatment.

Which One Is More Effective?
Let’s cut through the noise. A 2023 study from the National Center for Biotechnology Information looked at 151 patients - 77 on peritoneal dialysis and 74 on hemodialysis. The results were clear: PD patients had better blood pressure control, more stable heart rates, and lower levels of harmful hormones like parathyroid hormone. They also had fewer overall complications.
Why? Because hemodialysis is like a sudden flood - pulling out fluid and toxins in a few hours. That puts stress on your heart and blood vessels. It can cause cramps, dizziness, or even heart strain. Peritoneal dialysis is more like a slow drip. It removes waste gradually, so your body doesn’t get shocked. Studies show PD also does a better job of protecting any remaining kidney function you still have. That matters. Even a little bit of natural kidney function can improve your long-term survival.
But here’s the catch: hemodialysis removes waste faster per session. If you’ve just had a massive heart attack, severe fluid overload, or acute kidney injury, hemodialysis is the go-to. It’s the emergency tool. Peritoneal dialysis isn’t built for crisis. It’s built for steady, long-term management.
Side Effects and Risks
Both treatments come with risks - just different ones.
Hemodialysis risks include:
- Low blood pressure during sessions (affects nearly half of patients)
- Cramps and nausea from rapid fluid removal
- Vascular access problems - infections, clots, or failed fistulas
- Need for frequent trips to the clinic, which can disrupt work and life
Peritoneal dialysis risks include:
- Peritonitis - abdominal infection from contaminated exchanges (0.3-0.7 episodes per patient per year)
- Catheter blockage or leakage
- Weight gain from sugar in dialysate fluid
- Weakness from long-term use of glucose-based solutions damaging the peritoneal membrane
One major study found PD patients had 30% fewer hospitalizations overall compared to HD patients. But the fear of infection is real. Every time you connect a bag, you’re risking germs entering your belly. That’s why training is so critical. You can’t just wing it.
Quality of Life and Lifestyle Impact
Let’s talk about real life.
A 2022 survey by the National Kidney Foundation found 68% of peritoneal dialysis users reported higher satisfaction with treatment flexibility. Why? Because they weren’t tied to a clinic schedule. They could work, travel, or sleep in. One patient from Edinburgh told me, “I do my exchanges while watching TV at night. I don’t miss work. I don’t feel wiped out.”
But hemodialysis patients? 97% of those on Reddit’s r/kidneydisease forum said they hated the rigid schedule. 83% said they felt exhausted for hours after each session. Many said they couldn’t hold down jobs because they were too tired.
Peritoneal dialysis requires more personal responsibility. You need good eyesight, steady hands, and the ability to follow a strict hygiene routine. If you have arthritis, tremors, or vision problems, it might not be an option. Hemodialysis doesn’t ask you to do anything - the staff handles everything. You sit, you rest, you watch TV.
Cost-wise, PD is cheaper. The Journal of Peritoneal Therapy and Clinical Practice found PD provides better value for money. Less clinic use, fewer staff hours, fewer emergency visits. In the UK, about 22% of dialysis patients use PD - higher than the US (12%) because of better access and training.
Who Is Each Treatment Best For?
There’s no one-size-fits-all. But here’s a simple guide:
Choose hemodialysis if:
- You have severe heart problems or unstable blood pressure
- You’re older or have trouble managing daily tasks
- You don’t want to be responsible for sterile procedures
- You live far from a clinic but still want structured care
Choose peritoneal dialysis if:
- You want flexibility - to work, travel, or sleep normally
- You’re medically stable and have good manual dexterity
- You’re motivated to learn and follow a routine
- You want to protect your remaining kidney function
- You live in a place with good PD training (like the UK or Hong Kong)
There are exceptions. Some people start with PD and switch to HD if they get infections. Others start with HD and later move to PD when they’re ready for more independence. It’s not a one-time decision. Your needs change.
Future Trends and What’s Changing
Peritoneal dialysis is growing - slowly. The US is pushing hard to get more people on home dialysis. By 2025, the goal is for 80% of new patients to get education about home dialysis or transplant. Right now, only 12% of US patients use PD. But that’s changing. New dialysate solutions (like icodextrin) are reducing glucose damage and improving long-term outcomes. More nephrologists are being trained in PD techniques. And patients? They’re asking for it.
In the UK, PD adoption is rising. More clinics now offer training. More GPs understand the benefits. And patients? They’re choosing it because they want control over their lives.
The future of dialysis isn’t about which machine is better. It’s about matching the treatment to the person. Your kidneys are gone. But you’re still here. And you deserve a treatment that fits your life - not the other way around.
Can I switch from hemodialysis to peritoneal dialysis?
Yes, many people do. If you’re stable, have a good support system, and are willing to learn the technique, switching is possible. It usually requires a few weeks of training and a new catheter placement. Your care team will help you transition safely. Some patients switch because they want more freedom. Others switch after repeated infections or complications from vascular access.
Is peritoneal dialysis safer than hemodialysis?
It depends on what you mean by “safer.” PD has fewer risks to your heart and blood vessels because it’s gentler on your body. But it carries a higher risk of infection in the abdomen. Hemodialysis can cause sudden drops in blood pressure and heart strain. Neither is risk-free. PD is generally safer for long-term stability. HD is safer in emergencies. The best choice depends on your health, lifestyle, and ability to manage care.
Do I need to go to the hospital for peritoneal dialysis?
No, you don’t need to go to the hospital for regular treatments. All exchanges are done at home. But you will need to visit a clinic for initial catheter placement, training (usually 10-14 days), and regular checkups every few months. If you get an infection like peritonitis, you’ll need to go to the hospital for antibiotics. But day-to-day, it’s all done by you - no travel needed.
Can I travel with peritoneal dialysis?
Yes - and this is one of its biggest advantages. You can pack your dialysis fluid in a cooler and take it with you. Most airlines allow it as medical equipment. You can do exchanges in hotel rooms, at a friend’s house, or even outdoors if you have a clean space. Many patients travel internationally with PD. Hemodialysis requires booking appointments weeks in advance at dialysis centers abroad - and not all places have them.
Which treatment is more affordable?
Peritoneal dialysis is generally more cost-effective. It uses fewer clinic visits, less staff time, and fewer emergency interventions. A 2023 study found PD saved healthcare systems money while improving patient outcomes. In the UK and Canada, PD is often the first-line option for eligible patients because of its value. Hemodialysis costs more because it requires specialized equipment, trained staff, and facility space for every session.
Why isn’t peritoneal dialysis more widely used?
It’s not because it’s worse - it’s because it’s harder to teach. Many doctors weren’t trained in PD. Clinics are built for hemodialysis machines. Insurance systems in some countries pay more for in-center care. And patients are often told, “It’s easier to just come to the clinic.” But awareness is growing. In places like Hong Kong and the UK, PD is common because training and support are strong. The tide is turning - slowly.
