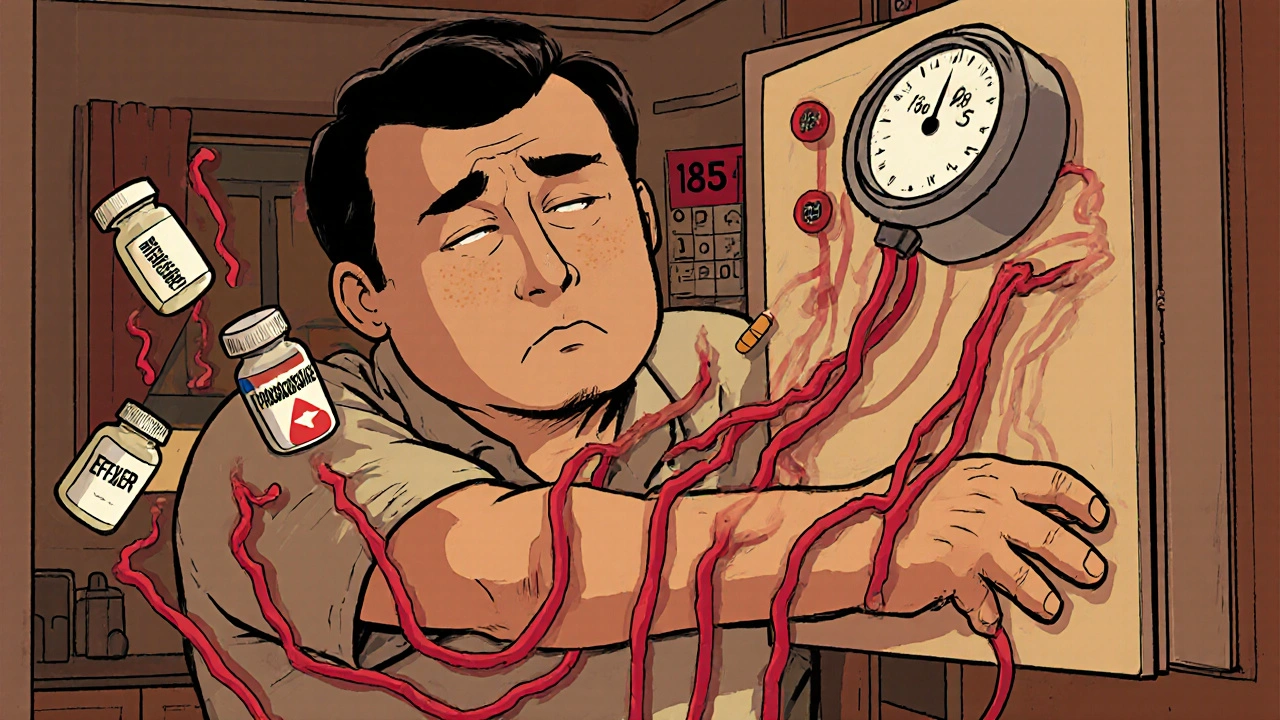
Many people don’t realize that the pills they take for pain, allergies, or depression could be quietly raising their blood pressure. It’s not just about aging or diet - sometimes, the cause is right in your medicine cabinet. Drug-induced hypertension affects millions, yet it’s often missed because the symptoms don’t show up until it’s too late. If you’re on regular medication and your blood pressure won’t budge despite lifestyle changes, it might not be your fault - it could be your meds.
What Medications Actually Raise Blood Pressure?
It’s not just illegal drugs or experimental treatments. Common, over-the-counter, and prescription medicines can push your blood pressure up. The biggest culprits? NSAIDs, corticosteroids, antidepressants, decongestants, and stimulants.Take ibuprofen, for example. It’s in Advil, Motrin, and countless generic brands. People use it for headaches, back pain, or menstrual cramps. But studies show that just two weeks of regular use can raise systolic blood pressure by 5 to 10 mm Hg in people who already have high blood pressure. That’s enough to push someone from controlled to uncontrolled hypertension. Naproxen is a bit gentler, but still risky if taken daily.
Corticosteroids like prednisone are even more powerful. If you’re taking 20 mg or more per day for more than four weeks, your chances of developing high blood pressure jump to 50-60%. That’s not a small risk - it’s a near certainty for many. The body holds onto sodium and water, blood volume increases, and pressure climbs fast. Some patients see spikes of 15 mm Hg within 24 hours.
Antidepressants like venlafaxine (Effexor) can also do damage. At doses above 150 mg/day, they increase norepinephrine levels by 300-400%, which tightens blood vessels and speeds up the heart. About 8-15% of users develop noticeable hypertension. Decongestants like pseudoephedrine (in Sudafed) cause immediate spikes - systolic pressure can rise 5-10 mm Hg within an hour and last up to 12 hours. Even one dose can be dangerous if you’re already hypertensive.
Stimulants for ADHD, like Adderall or Ritalin, raise BP in 10-25% of users. Erythropoietin (used for anemia) and some HIV drugs also carry significant risk. And don’t forget herbal supplements - St. John’s Wort, for instance, has been linked to hypertensive crises in people on other medications.
How Do These Drugs Actually Raise Blood Pressure?
It’s not magic - it’s physiology. Each drug works differently, but they all end up doing the same thing: making your blood vessels tighter or your body hold onto more fluid.NSAIDs block enzymes that help your kidneys get rid of sodium. Without those enzymes, you retain water. Your blood volume goes up. Your heart has to pump harder. That’s why ibuprofen reduces kidney blood flow by 15-20% within two hours.
Corticosteroids mimic aldosterone, a hormone that tells your kidneys to hold onto salt and dump potassium. More salt means more fluid. One study found that 30 mg of prednisone per day increases plasma volume by 10% in just three days.
Decongestants activate alpha-receptors in blood vessel walls. This causes immediate vasoconstriction - your arteries narrow. Pseudoephedrine increases peripheral resistance by 25-30% in under an hour.
Antidepressants like SNRIs prevent your brain from reabsorbing norepinephrine. That leaves more of it floating around, which keeps your sympathetic nervous system revved up. Your heart beats faster. Your vessels constrict. Pressure climbs.
It’s not one mechanism - it’s a cascade. And if you’re taking more than one of these drugs, the effects add up. That’s why so many people with “resistant hypertension” are actually just on too many BP-raising meds.
How to Monitor Your Blood Pressure Correctly
If you’re on any of these medications, don’t wait for symptoms. High blood pressure doesn’t cause headaches or dizziness until it’s already damaging your heart, kidneys, or brain.Start with a baseline reading before you begin any new medication. Then check again at 1-2 weeks, 4-6 weeks, and every 3 months after that. If you’re on corticosteroids, check daily for the first month. Look for orthostatic changes - if your standing BP is 20 mm Hg higher than your sitting BP, that’s a red flag.
Home monitoring is key. Measure twice a day for seven days before starting a new drug, and again after any dose change. Use the average of the second six days. Don’t rely on one-off readings at the doctor’s office - they can be misleading due to white-coat hypertension.
For high-risk patients - those with kidney disease, existing hypertension, or on multiple BP-raising drugs - ambulatory blood pressure monitoring (ABPM) is the gold standard. It tracks your pressure over 24 hours. A daytime average above 135 mm Hg or a 24-hour average above 130 mm Hg confirms drug-induced hypertension.
And here’s the hard truth: most doctors don’t ask about OTC meds. A 2023 study found only 22% of primary care providers routinely screen for NSAID use in hypertensive patients. Don’t wait for them to ask. Bring your full list - pills, patches, creams, supplements, even cough syrups - to every appointment.
How to Manage It - Step by Step
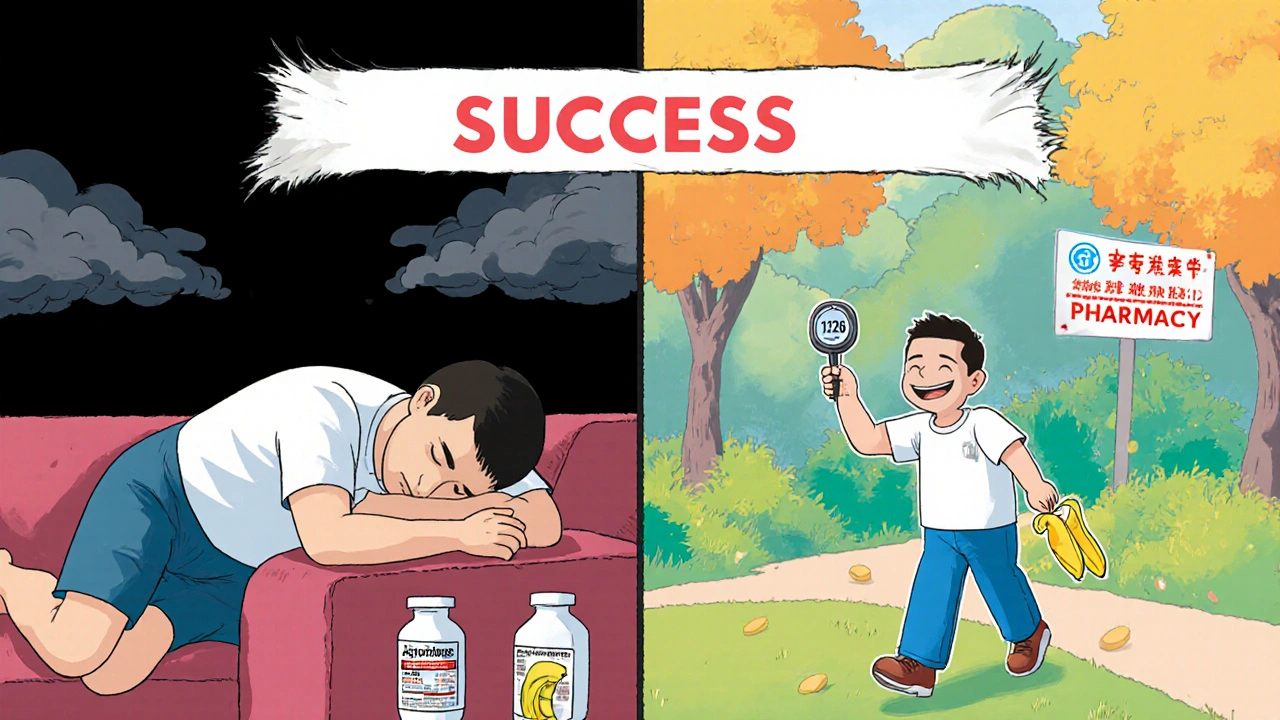
The good news? Drug-induced hypertension often reverses once you stop or switch the offending medication.Step 1: Review your meds. Sit down with your doctor and list everything you take - even the “harmless” ones. Look for NSAIDs, decongestants, stimulants, or steroids. If you’re taking two or more BP-raising drugs, that’s a major risk factor.
Step 2: Replace when possible. For pain, try acetaminophen (up to 3,000 mg/day) instead of ibuprofen. For congestion, use saline sprays or antihistamines like loratadine instead of pseudoephedrine. For depression, SSRIs like sertraline tend to have less BP impact than SNRIs.
Step 3: Don’t quit steroids cold turkey. If you’re on prednisone for lupus, rheumatoid arthritis, or another chronic condition, don’t stop without medical help. Instead, work with your doctor to lower the dose gradually while adding a blood pressure medication.
Step 4: Use the right BP drugs. Not all antihypertensives work the same here. Beta-blockers? They’re often ineffective because they don’t fix vasoconstriction. Calcium channel blockers like amlodipine or thiazide diuretics like hydrochlorothiazide are first-line choices. In 35-45% of cases, you’ll need both.
Step 5: Add lifestyle tweaks. Cut sodium to under 1,500 mg a day. Eat potassium-rich foods - bananas, spinach, sweet potatoes. Get 150 minutes of walking or cycling weekly. These changes can drop your BP by 5-8 mm Hg - enough to bring you back into range.
What Doesn’t Work - And Why
Many people try to treat high blood pressure with the same tools they’d use for essential hypertension. That’s a mistake.Beta-blockers are commonly prescribed, but they’re not ideal for drug-induced cases. A 2022 trial showed only a 45% response rate compared to 72% for calcium channel blockers. Why? Because beta-blockers slow the heart, but they don’t relax constricted vessels - the real problem with NSAIDs, decongestants, and steroids.
Also, don’t assume your doctor knows. A 2022 JAMA study found only 58% of physicians could correctly identify all 12 high-risk medication classes. Most don’t realize that a single Advil a day can undo months of blood pressure control.
And never ignore herbal supplements. St. John’s Wort, licorice root, ginseng - they’re not “natural” in the safe sense. They interact with your body’s systems in unpredictable ways. One patient’s hypertensive crisis was traced back to a daily tea made from licorice root.
Real Stories, Real Consequences
Online forums are full of people who didn’t know their meds were the problem.One Reddit user took ibuprofen daily for arthritis for five years. His BP hovered around 150/95. His doctor kept increasing his blood pressure meds. He was on four drugs. Then he switched to acetaminophen. Within three weeks, his BP dropped to 120/78 - and he got off two of the pills.
A 68-year-old woman in Ohio was diagnosed with “resistant hypertension.” She was on three medications. Her BP never came down. Her pharmacist noticed she was taking Sudafed every morning for allergies. She switched to a non-decongestant allergy pill. Her systolic pressure fell 22 points in 21 days.
On the flip side, many patients report frustration. One Healthgrades review said it took 8.7 months to get the right diagnosis. Another said her doctor dismissed her concerns: “It’s just stress.”
These aren’t rare cases. A 2023 study found that 15-20% of people referred for resistant hypertension had drug-induced causes - and most were on NSAIDs or decongestants.
What’s Changing - And What You Should Know
The medical world is waking up. The FDA now requires stronger warnings on NSAID labels. The European Medicines Agency updated corticosteroid guidelines in 2023. The American Heart Association has launched a $8.5 million research push to improve detection.Tools like the American College of Cardiology’s Drug-Induced Hypertension Calculator are now available to help doctors input your meds and get a risk score. Clinical trials are testing pharmacist-led medication reviews - early results show a 28% drop in uncontrolled BP among patients who got these reviews.
But progress is slow. Only 38% of U.S. hospitals have formal screening protocols. Most patients still fall through the cracks.
Your job? Be your own advocate. Keep a written list of every medication you take. Ask your doctor: “Could any of these be raising my blood pressure?” If they don’t know, ask for a referral to a hypertension specialist. Don’t let a simple oversight cost you your long-term health.
Final Thoughts
High blood pressure from medication isn’t your fault. It’s a hidden side effect that’s been overlooked for decades. But it’s fixable - if you catch it early.You don’t need to stop your essential meds. You just need to know which ones are hurting you and how to swap, adjust, or manage them safely. With the right monitoring and a few smart changes, you can take back control - without adding more pills to your routine.
Can over-the-counter painkillers like ibuprofen really raise blood pressure?
Yes. Regular use of ibuprofen (Advil, Motrin) can raise systolic blood pressure by 5-10 mm Hg in people with existing hypertension. Studies show about 12% of hypertensive patients experience clinically significant spikes after two weeks of use. Naproxen (Aleve) has a smaller effect, but still carries risk with daily use. Acetaminophen (Tylenol) is a safer alternative for pain relief.
How long does it take for blood pressure to drop after stopping a medication that causes hypertension?
It varies by drug. For NSAIDs and decongestants, blood pressure often drops within 2-4 weeks after stopping. Corticosteroids may take longer - up to 6-8 weeks - because the body needs time to reset its fluid balance. Antidepressants like venlafaxine can show improvement in 1-3 weeks. Always taper off under medical supervision, especially with steroids.
Are herbal supplements safe for people with high blood pressure?
Not always. St. John’s Wort, licorice root, ginseng, and ephedra-containing products can significantly raise blood pressure or interfere with BP medications. One patient had a hypertensive crisis after drinking licorice tea daily for months. Always tell your doctor about supplements - they’re not regulated like prescription drugs and can be just as dangerous.
Why aren’t doctors always warning patients about this?
Many physicians aren’t trained to recognize drug-induced hypertension as a common cause of treatment-resistant high blood pressure. A 2022 study found only 58% of doctors could correctly identify all 12 high-risk medication classes. Plus, patients rarely mention OTC or herbal use unless asked directly. The problem is systemic - not personal.
What’s the best blood pressure medication for drug-induced hypertension?
Calcium channel blockers like amlodipine and thiazide diuretics like hydrochlorothiazide are first-line choices. They work directly on the mechanisms causing the rise - relaxing blood vessels and reducing fluid volume. Beta-blockers are less effective because they don’t address vasoconstriction, which is the main issue with NSAIDs, decongestants, and steroids.
Should I stop my medication if my blood pressure goes up?
Never stop a prescribed medication without talking to your doctor. For example, stopping prednisone suddenly can cause adrenal crisis. Instead, schedule a medication review. Your doctor may lower the dose, switch to a safer alternative, or add a blood pressure medication. The goal is to treat the cause - not just the symptom.
Can lifestyle changes help reverse medication-induced high blood pressure?
Yes. Reducing sodium to under 1,500 mg per day, increasing potassium intake (2,500-3,500 mg/day), and doing 150 minutes of moderate exercise weekly can lower blood pressure by 5-8 mm Hg. These changes support your body’s natural ability to regulate pressure and make medications more effective - even if you can’t stop the offending drug.
Kat Sal
October 30, 2025 AT 05:03OMG I had no idea my daily ibuprofen for back pain was doing this to me. I’ve been on three different BP meds and nothing worked. Switched to Tylenol last month and my numbers dropped like a rock. My doctor was shocked. You’re not broken-you’re just on the wrong pills.
Share this with everyone you know. This needs to be common knowledge.
Rebecca Breslin
October 31, 2025 AT 15:45Let me guess-you’re one of those people who thinks all meds are poison and herbs are magic. NSAIDs raise BP? Shocking. So is gravity. The real issue is that lazy doctors don’t check med histories. I’ve seen patients on 12 different drugs and no one bothered to ask if they were taking Sudafed for a cold. It’s not the meds-it’s the lack of coordination.
And yes, I’m a pharmacist. No, I don’t get paid to say this. I just care.
Kierstead January
November 1, 2025 AT 10:09Of course your meds are raising your BP. You’re American. You pop pills like candy. You take Advil for a stubbed toe. You take prednisone for a sneeze. You drink licorice tea because ‘it’s natural.’
Stop blaming the system. Stop blaming the doctors. You’re the problem. You want a quick fix for everything, then wonder why your body’s falling apart.
My grandma didn’t have BP meds. She didn’t need them. She didn’t take 17 pills a day. Maybe try not being a medical trainwreck for once?
Imogen Levermore
November 1, 2025 AT 20:57…but what if the FDA is lying? 🤔
Ever notice how every time someone figures out meds cause hypertension, the pharma giants quietly fund ‘research’ that says ‘nope, it’s stress’?
They don’t want you to know that your ‘essential hypertension’ is actually your ibuprofen + antidepressant + decongestant combo.
They want you on lifelong meds.
Also, I think the moon is made of cheese. But that’s just me. 🌕🧀
Chris Dockter
November 2, 2025 AT 03:14Gordon Oluoch
November 2, 2025 AT 18:45The real tragedy isn’t drug-induced hypertension. It’s the moral decay of a society that treats symptoms like commodities. You don’t fix a leaky pipe by adding more water. You fix the pipe.
But no-people want a pill for the pill. A pill to undo the pill. You’ve outsourced your responsibility to Big Pharma and your GP who has 8 minutes per patient.
And now you’re surprised your kidneys are failing?
This isn’t medicine. It’s corporate theater.
Tyler Wolfe
November 4, 2025 AT 12:58Just wanted to say thank you for this. I’m 52 and have had high BP since 40. My doc kept upping my meds. I felt awful. Then I mentioned I took ibuprofen for my knees every day. He said ‘oh’ and we switched me to naproxen, then acetaminophen. My BP dropped 15 points. I didn’t even need to change my diet.
Just ask the question. Bring your list. You’re not being annoying-you’re saving your life.
Neil Mason
November 5, 2025 AT 05:10As a Canadian, I’m kinda shocked this isn’t more widely known here too. We’re not immune. My aunt took OTC painkillers for years after her hip surgery. Her BP went through the roof. Her pharmacist caught it. We switched her to physical therapy + Tylenol. Her BP normalized in 6 weeks.
Side note: I think we need more pharmacist-led med reviews. They see the whole picture. Docs are busy. Pharmacists? They’re the ones who actually read the labels.
Andrea Gracis
November 6, 2025 AT 23:43Matthew Wilson Thorne
November 8, 2025 AT 23:40April Liu
November 9, 2025 AT 03:00You’re not alone. I’ve been where you are. Took me 3 years and 4 doctors to figure out my antidepressant was the problem.
Here’s what helped me:
1. Wrote down every pill, supplement, and cough syrup I took.
2. Printed the list. Gave it to my doc before every visit.
3. Asked: ‘Could any of these be raising my BP?’
My BP dropped 20 points after switching meds. I didn’t need more pills-I needed better info.
You’ve got this. And you’re not crazy. 💪❤️