For millions of women entering menopause, the sudden wave of hot flashes, sleepless nights, and brain fog doesn’t just feel inconvenient-it can feel like losing control of your own body. Hormone Replacement Therapy (HRT) isn’t a magic fix, but for many, it’s the most effective tool available to regain stability. Yet, after decades of mixed messages, fear, and confusion, it’s no wonder so many women hesitate. Is HRT safe? Does it really work? And how do you know if it’s right for you? The answer isn’t a simple yes or no. It’s about timing, type, and tracking.
What HRT Actually Does
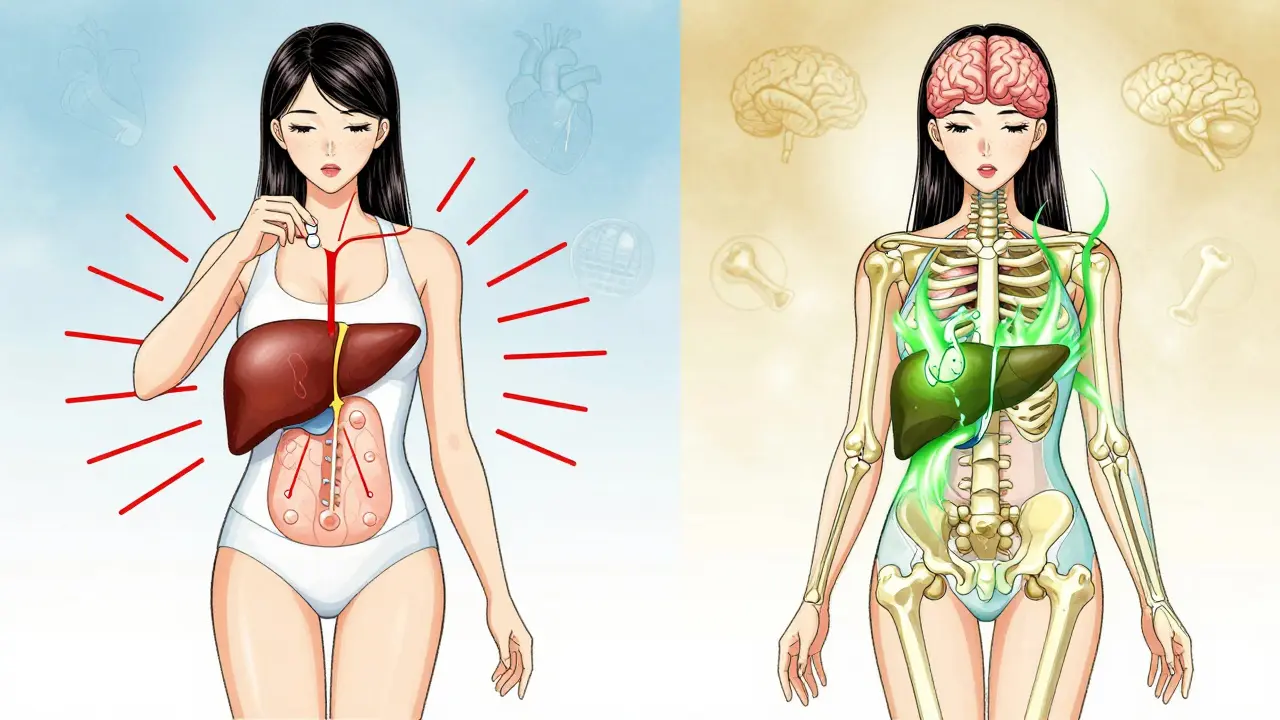
HRT replaces the estrogen (and sometimes progesterone) your body stops making after menopause. It’s not about slowing aging-it’s about managing symptoms caused by hormone loss. The most common symptoms it helps? Hot flashes and night sweats. Studies show HRT reduces these by 80-90%, far more than antidepressants like SSRIs, which only cut them by about half. It also helps with vaginal dryness, mood swings, and prevents bone loss that leads to fractures.
There are two main types: estrogen-only therapy (ET) for women who’ve had a hysterectomy, and estrogen-progestogen therapy (EPT) for those with a uterus. Without progesterone, estrogen can cause the uterine lining to thicken dangerously, raising cancer risk. So if you still have your uterus, you need both.
Delivery matters too. You can take HRT as pills, patches, gels, vaginal rings, or even implants. Oral pills are common, but they go through your liver first, which increases the risk of blood clots. Transdermal options-patches and gels-bypass the liver and are now preferred for most women because they carry about 1.5 to 2 times less risk of deep vein thrombosis. For example, transdermal estrogen causes about 1.3 clots per 1,000 women per year; oral causes 3.7.
The Real Benefits: More Than Just Hot Flashes
Yes, HRT is the gold standard for hot flashes. But its benefits go deeper. The Women’s Health Initiative (WHI) found HRT reduces the risk of osteoporotic fractures by 34%. That’s more than what most bone drugs like bisphosphonates offer in the first few years. For women in their 50s, this isn’t just about comfort-it’s about staying independent as they age.
Heart health is another big piece. When HRT starts before age 60 or within 10 years of menopause, it lowers the risk of coronary heart disease by 32%. That’s according to NAMS guidelines updated in 2022. But start it later, and that benefit disappears. In fact, starting after 60 may slightly raise heart attack risk. This is called the “timing hypothesis,” and it’s the most important rule in modern HRT.
And yes, it helps with brain fog. Many women report clearer thinking, better focus, and improved sleep-not because HRT is a nootropic, but because when you stop waking up drenched in sweat every two hours, your brain gets the rest it needs to function.
The Risks: What You Need to Know
Let’s be clear: HRT isn’t risk-free. The biggest concern is breast cancer. The WHI study found a 26% higher risk with EPT after 5.6 years. But here’s what most people miss: that’s 8 extra cases per 10,000 women per year. For context, the average woman’s lifetime risk of breast cancer is about 13%. HRT adds a small bump, not a tsunami.
For women with a personal history of breast cancer, HRT is off-limits. Same goes for those with a history of blood clots, stroke, or unexplained vaginal bleeding. If you’re over 60 and have never used HRT before, it’s usually not recommended.
Another risk is stroke. Oral estrogen increases stroke risk by about 30%. Transdermal doesn’t. That’s why many doctors now start with patches or gels-especially for women with high blood pressure or a family history of clots.
Then there’s the myth of “bioidentical” hormones. Compounded bioidenticals-marketed as “natural” and “safer”-aren’t FDA-approved, aren’t tested for safety, and aren’t proven to be better than standard HRT. The Endocrine Society says there’s no evidence they reduce risk. In fact, they can be more dangerous because dosing isn’t standardized.
Monitoring: How to Stay Safe on HRT
You don’t start HRT and forget about it. Monitoring is non-negotiable. Before you begin, you need a baseline mammogram, blood pressure check, pelvic exam, and BMI measurement. No exceptions.
After three months, you come back. That’s when most side effects show up-breast tenderness, bloating, mood swings, or irregular bleeding. If bleeding lasts longer than six months, you need an endometrial biopsy. It’s common in the first few months, but not normal past that point.
After that, annual visits are standard: blood pressure, weight, breast exam, and a check-in on symptoms. No one wants to hear “come back in a year,” but skipping this puts you at risk. Many women stop HRT because they’re scared-not because it’s failing, but because no one explained what to expect.
Some clinics now use genetic testing to personalize dosing. Variants in the CYP1B1 gene affect how quickly your body breaks down estrogen. If you’re a slow metabolizer, lower doses work better and cause fewer side effects. It’s not standard yet, but it’s coming.
What HRT Isn’t
HRT won’t make you look younger. It won’t fix wrinkles or restore your libido (though better sleep and less discomfort can help). It’s not a substitute for exercise, calcium, or vitamin D. It’s not for women who just want to feel “like their 30s again.”
It’s also not a one-size-fits-all. A 52-year-old woman with severe hot flashes and no family history of breast cancer? HRT is likely a great fit. A 65-year-old woman with high blood pressure and a history of clots? Not even close.
And it’s not forever. Most women use HRT for 3-5 years, just long enough to get through the worst of menopause. Some stay longer if symptoms persist and risks remain low. But the goal is always the lowest dose for the shortest time.

Real Stories, Real Choices
One woman, 54, started transdermal estradiol after months of sleepless nights and panic attacks. Within six weeks, she could sleep through the night. Within three months, she was hiking again. She’s been on it for four years. Her mammograms are normal. Her blood pressure is stable. She checks in every year.
Another, 58, tried oral HRT and got a blood clot. She switched to a patch. No more clots. Her hot flashes are gone. She’s now on a low-dose regimen and feels like herself again.
Then there are the ones who quit. Thirty-five percent of women stop HRT within a year. Why? Fear of breast cancer (48%), bleeding (22%), or nausea (12%). But here’s the thing: those who switch from oral to transdermal report fewer side effects and higher continuation rates. The problem isn’t HRT-it’s the wrong type, the wrong dose, or no follow-up.
Where HRT Stands Today
In 2026, HRT is no longer the villain it was after 2002. The FDA removed its black box warnings in 2022 after reviewing new data. The message now is clear: for healthy women under 60 or within 10 years of menopause, the benefits outweigh the risks.
Prescriptions are rising again. In the U.S., 12-18% of menopausal women now use HRT-up from a low of 9 million prescriptions in 2003 to 15.7 million in 2022. Europe is ahead, with 22-28% usage. The market is growing, not because of marketing, but because doctors are finally listening to the science.
New options are on the horizon. TSECs like Duavee combine estrogen with a drug that protects the uterus, cutting endometrial thickening risk by 76%. Transdermal progesterone is being tested to avoid the side effects of oral progestogens. And personalized dosing based on genetics is moving from research labs into clinics.
The bottom line? HRT isn’t for everyone. But for the right woman, at the right time, with the right monitoring, it’s one of the most effective, life-improving treatments in modern medicine.
Is hormone replacement therapy safe for women over 60?
HRT is generally not recommended for women over 60 who haven’t used it before. Starting HRT at this age increases the risk of stroke, blood clots, and possibly heart disease. If you started HRT before 60 and are doing well, you may continue under close monitoring-but starting new after 60 is rarely advised.
Does HRT cause breast cancer?
Combined HRT (estrogen + progestogen) slightly increases breast cancer risk-about 8 extra cases per 10,000 women per year. That’s a small increase compared to the overall lifetime risk of 13%. Estrogen-only therapy doesn’t raise the risk in women without a uterus. Risk goes up the longer you use it, but drops after you stop. Transdermal HRT may carry lower risk than oral. Always discuss your personal risk factors with your doctor.
What’s better: pills or patches?
Patches and gels (transdermal) are safer than pills for most women. They don’t pass through the liver first, so they’re less likely to cause blood clots or raise blood pressure. They’re also more stable in the body, leading to fewer mood swings. Pills are still used, especially if cost or access is an issue, but transdermal is now the preferred first choice for healthy women.
Can I use HRT if I have a family history of breast cancer?
It depends. If you have a BRCA mutation or a strong family history, estrogen-only therapy (if you’ve had a hysterectomy) may be safer than combined HRT. But you’ll need a detailed risk assessment with a specialist. Some women with family history can still use HRT safely with close monitoring-others should avoid it. Genetic counseling and regular screenings are essential.
How long should I stay on HRT?
Most women use HRT for 3-5 years to get through the worst of menopause symptoms. Some need it longer if symptoms persist and their health profile allows it. The goal is always the lowest effective dose for the shortest time. There’s no fixed deadline-regular check-ins with your doctor will guide when to taper off.
Are bioidentical hormones safer than traditional HRT?
No. Compounded “bioidentical” hormones aren’t FDA-approved, aren’t tested for safety, and aren’t proven to be safer. They’re often marketed as “natural,” but they carry the same risks as standard HRT. The Endocrine Society and FDA both state there’s no evidence they reduce side effects or cancer risk. Stick with FDA-approved products for predictable dosing and safety monitoring.
What if I have irregular bleeding on HRT?
Irregular bleeding is common in the first 3-6 months, especially with cyclical progestogen. But if it lasts longer than six months, you need an evaluation. Persistent bleeding can signal endometrial changes. Your doctor may adjust your dose, switch to continuous progestogen, or order an ultrasound or biopsy. Don’t ignore it-rule out serious causes.
Can HRT help with memory or prevent dementia?
HRT doesn’t prevent dementia. In fact, starting it after age 65 may slightly increase dementia risk. But for women who start it early-before 60-it may support brain health by improving sleep, reducing stress, and stabilizing mood. Better sleep and less brain fog can make you feel sharper, but HRT isn’t a cognitive enhancer.
Next Steps: What to Do Now
If you’re considering HRT, start by tracking your symptoms. How bad are your hot flashes? Are you sleeping? Is your mood affected? Write it down.
Then, find a provider who knows current guidelines. Ask: “Do you follow NAMS or Endocrine Society recommendations?” If they mention “bioidenticals” as a miracle cure, walk away. Look for someone who talks about timing, delivery methods, and monitoring-not just prescriptions.
Request a baseline mammogram and blood pressure check. Don’t skip the pelvic exam. If you’re under 60 and have moderate-to-severe symptoms, HRT could be the key to getting your life back. But only if it’s done right.

Juan Reibelo
January 23, 2026 AT 21:14Transdermal patches are the way to go-no liver stress, lower clot risk, and you don’t feel like you’re on a hormonal rollercoaster every other day. I’ve seen patients switch from pills and immediately sleep through the night. It’s not magic, it’s physiology.
Jamie Hooper
January 24, 2026 AT 07:33bioidentical my ass 😂 i got prescribed some ‘natural’ cream from a wellness blog and my boobs felt like they were gonna explode. switched to a patch and now i’m chillin’. why do people trust some guy in a yoga pants selling hormones on instagram?
Husain Atther
January 24, 2026 AT 21:49This is one of the most balanced and scientifically grounded explanations of HRT I’ve read in years. The emphasis on timing, delivery method, and monitoring is critical. Many women are denied relief due to outdated fears, while others are overprescribed without proper follow-up. A thoughtful approach saves lives.
Izzy Hadala
January 26, 2026 AT 07:45Given the data from the 2022 NAMS guidelines and the reanalysis of WHI subgroups, the risk-benefit profile for women initiating HRT under 60 and within 10 years of menopause is overwhelmingly favorable for symptom relief and long-term skeletal health. The 26% relative increase in breast cancer risk with EPT must be contextualized against the absolute risk increase of 0.08% per annum, which remains below the baseline risk associated with obesity or alcohol consumption.
Elizabeth Cannon
January 28, 2026 AT 00:53my mom was on pills for 2 years and got a clot. now she’s on a patch and says she feels like herself again. why do doctors still push oral first?? it’s not 2002 anymore. also, if you’re scared of breast cancer, get a mammogram and a genetic screen-not a panic attack.
Don Foster
January 28, 2026 AT 21:05Let’s be real most women who complain about HRT haven’t even read the WHI papers. They just saw a headline from 2002 and thought ‘oh god estrogen kills’ and now they’re stuck in menopause hell. The science has moved on. Your grandma’s fear isn’t your medical advice.
Phil Maxwell
January 29, 2026 AT 20:20just wanted to say thanks for this. i’ve been thinking about HRT for months but was too scared to ask my doctor. this broke it down so clearly. i’m gonna make an appointment next week.
Tommy Sandri
January 31, 2026 AT 19:00In Japan, HRT uptake remains below 5%, largely due to cultural perceptions of menopause as a natural transition to be endured rather than treated. This contrasts sharply with the U.S. and Northern Europe, where clinical intervention is normalized. The divergence reflects broader societal attitudes toward aging and medicalization.
Karen Conlin
February 1, 2026 AT 18:00Listen. If you’re 55 and your hot flashes are making you cry at your kid’s soccer game, you deserve relief. HRT isn’t vanity-it’s dignity. And if your doctor won’t talk to you about patches or timing, find a new one. You’re not asking for a miracle-you’re asking for your brain to stop screaming from lack of sleep. That’s not weak. That’s human.
asa MNG
February 2, 2026 AT 00:12OMG YES I WAS ON ORAL AND GOT A CLOT 😭 then i switched to patch and now i can finally drive without sweating through my shirt 🥲 also my husband says i stopped yelling at him every 5 minutes 🤣 bioidenticals are just snake oil with a fancy label
Sushrita Chakraborty
February 2, 2026 AT 22:25The assertion that transdermal estrogen reduces venous thromboembolism risk by 50% compared to oral formulations is supported by multiple meta-analyses, including those published in The Lancet and JAMA Internal Medicine. The pharmacokinetic advantage lies in the avoidance of first-pass hepatic metabolism, which minimizes hepatic synthesis of clotting factors. Furthermore, the Endocrine Society’s 2022 Clinical Practice Guideline explicitly recommends transdermal estrogen as the preferred route for women with cardiovascular risk factors. It is imperative that clinicians adhere to evidence-based guidelines rather than historical biases.