What Are Kyphoplasty and Vertebroplasty?
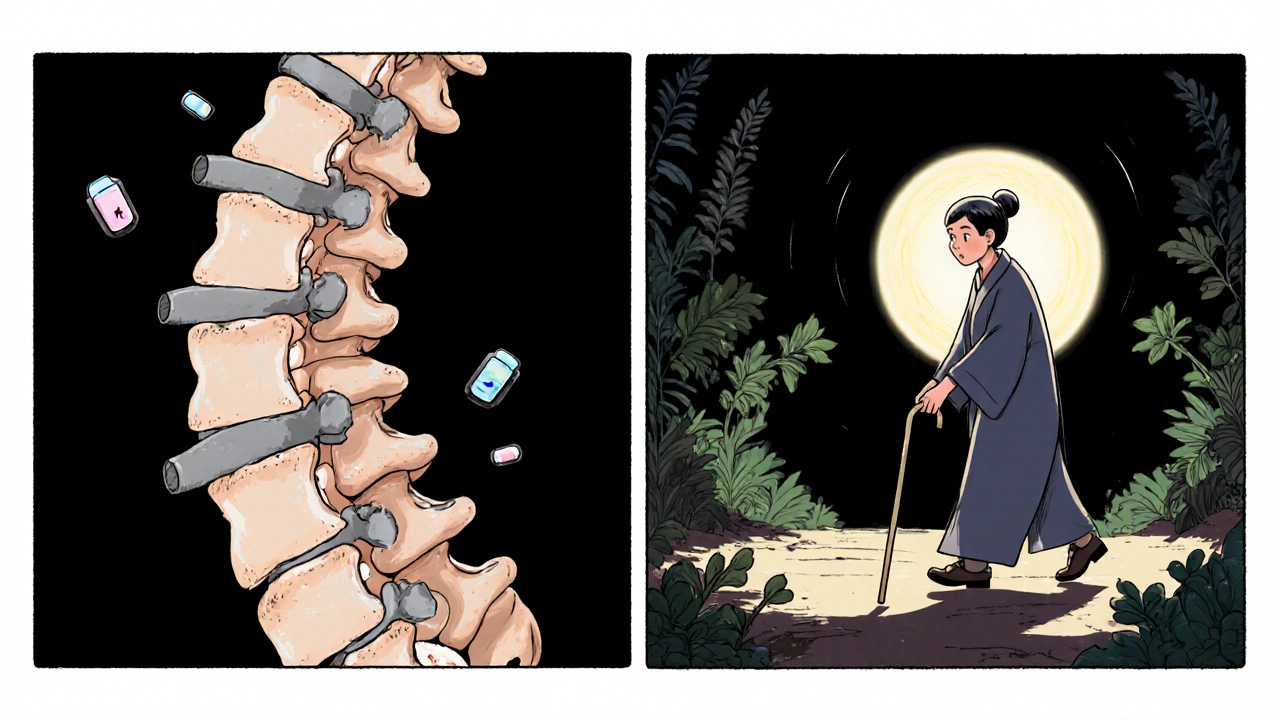
When a vertebra in your spine collapses-often from osteoporosis, injury, or cancer-it can cause severe pain, loss of height, and a hunched posture. These fractures are common, especially in people over 65. For many, painkillers and rest don’t help enough. That’s where kyphoplasty and vertebroplasty come in. Both are minimally invasive procedures that use medical-grade bone cement to stabilize the broken vertebra and bring quick pain relief. They’re not surgeries in the traditional sense. No large incisions. No long hospital stays. Most people go home the same day.
How Do They Work?
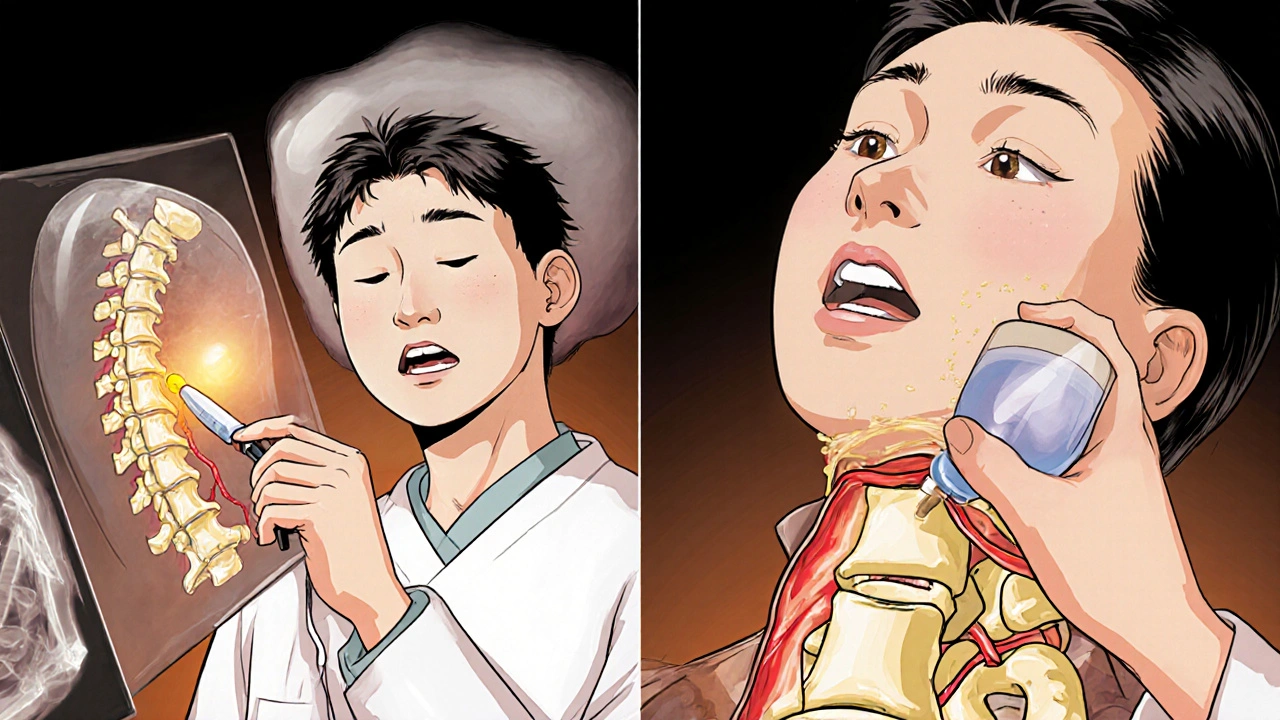
Both procedures start the same way: you lie face down, get local anesthesia with sedation, and a thin needle is guided into the fractured vertebra using real-time X-ray imaging. Then comes the difference.
In vertebroplasty, bone cement (polymethylmethacrylate or PMMA) is injected directly into the broken bone under pressure. The cement hardens in 10-20 minutes, acting like an internal cast. It stops the fracture from moving, which is what causes the pain.
In kyphoplasty, there’s an extra step. Before injecting cement, a small balloon is inserted into the fractured vertebra and gently inflated. This lifts the collapsed bone back toward its normal shape and creates a cavity inside. Then the balloon is popped, and cement is pumped into the space it left behind. The goal isn’t just to stop pain-it’s to restore some of the height you lost.
Which One Is Better for Pain Relief?
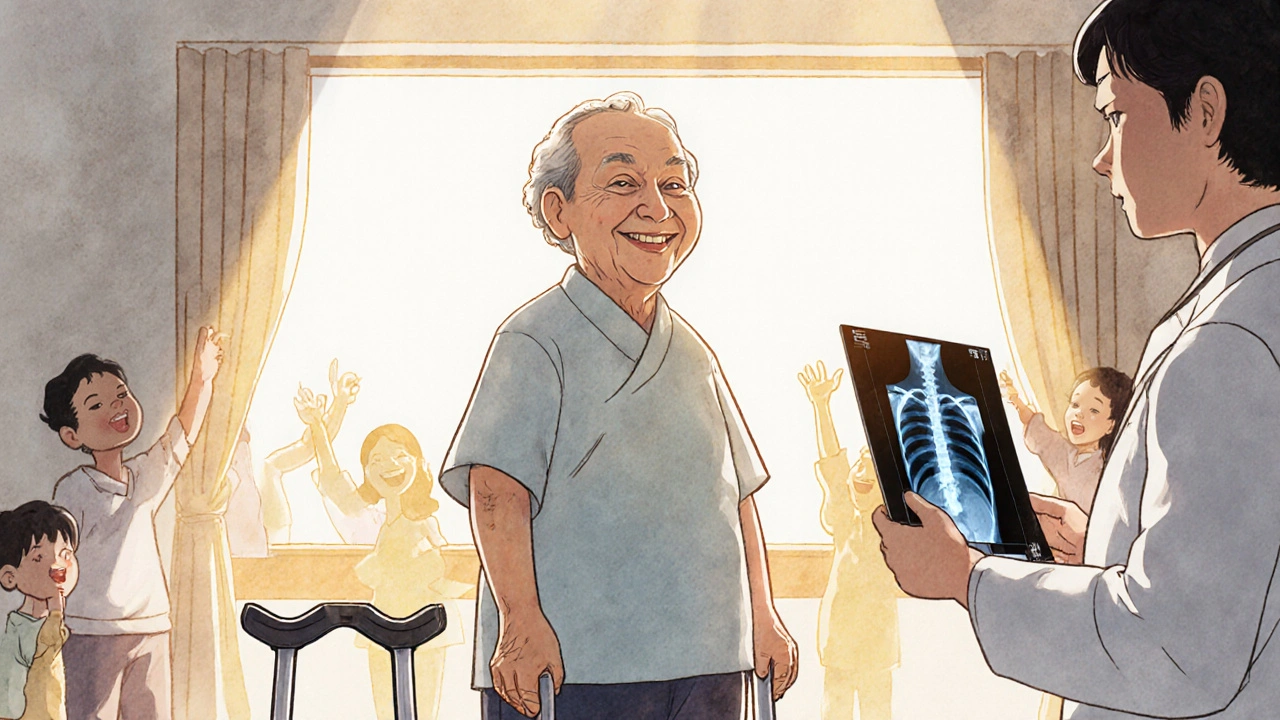
Here’s the surprising part: both procedures work almost equally well for pain. Studies show 85-90% of patients report a dramatic drop in pain within 24 hours. Before the procedure, average pain scores (on a scale of 0-10) are around 8.2. After? They drop to 1.5. That’s not a small change-it’s life-altering.
One patient on a chronic pain forum described it like flipping a switch: “I went from 9/10 pain to 2/10 in hours.” Another said their vertebroplasty didn’t fix their hunched back, but the pain? Gone. That’s the pattern. Both work for pain. The real difference isn’t in how you feel right away-it’s in what happens to the bone itself.
Height Restoration: Kyphoplasty’s Claim to Fame
Kyphoplasty was developed to fix more than just pain. It was designed to correct the spinal deformity that often comes with compression fractures-the stooped posture, the lost height, the way your clothes don’t fit anymore.
Studies show kyphoplasty can restore 40-60% of the lost height in the vertebra. Vertebroplasty? Almost none. That sounds like a big win. But here’s the catch: that restored height doesn’t always last. A 2007 study found that after just 500 normal body movements (like walking or standing), about 30% of the height gained in kyphoplasty was lost again. The bone doesn’t magically become strong again-it’s just held in place by cement.
So if your main goal is to look taller or stand straighter, kyphoplasty might help. But if you just want to stop the pain, vertebroplasty does the job just as well.
Complications and Risks
No procedure is risk-free. The biggest concern with both is cement leaking out of the bone. In vertebroplasty, leaks happen in 27-68% of cases. In kyphoplasty? Only 9-33%. Why? Because the balloon creates a controlled space for the cement to fill, reducing pressure and the chance it’ll escape into nearby tissues or blood vessels.
Most leaks cause no symptoms. But if cement leaks into the spinal canal or nerves, it can cause numbness, weakness, or even paralysis-though this is rare. Symptomatic complications occur in about 1.1% of vertebroplasty cases and 0.6% of kyphoplasty cases.
Another risk is new fractures in nearby vertebrae. About 5-10% of patients develop another fracture within a year. This isn’t because the procedure caused it-it’s because osteoporosis is still active. The bone around the treated area is weak, and the treated vertebra is now stiffer, shifting stress to its neighbors.
Cost and Accessibility
Kyphoplasty costs about 20-30% more than vertebroplasty. In 2023, Medicare paid $3,850 for kyphoplasty and $2,950 for vertebroplasty. The price difference comes from the balloon devices, which are expensive. But here’s the thing: most insurance, including Medicare, covers both if you’ve tried conservative treatments first-like bracing, physical therapy, and pain meds-for at least 4-6 weeks.
Because of the higher cost and similar pain outcomes, some experts argue vertebroplasty offers better value for patients without major spinal deformity. Others say kyphoplasty’s lower complication rate justifies the extra cost, especially for older patients with fragile bones.
Who Gets Which Procedure?
There’s no one-size-fits-all answer, but doctors use a few simple rules:
- If your fracture is recent (less than 8 weeks), shows swelling on MRI, and you have severe pain that hasn’t improved with rest or meds-you’re a candidate for either.
- If you’ve lost more than 30% of your vertebra’s height or have a noticeable hunchback, kyphoplasty is usually preferred.
- If your fracture is stable, the bone isn’t collapsed much, and you just need pain relief, vertebroplasty is often enough.
- If you’re over 80, have severe osteoporosis, or are at higher risk for bleeding or infection, vertebroplasty’s simpler technique may be safer.
Most procedures are done by interventional radiologists or spine surgeons who’ve completed at least 15-20 supervised cases. Kyphoplasty has a slightly steeper learning curve-surgeons often need 25 cases to feel confident with the balloon technique.
What Happens After the Procedure?
You’ll spend 4-6 hours in recovery, lying flat so the cement doesn’t shift. Most people walk the same day. You’ll be told to avoid heavy lifting or twisting for 24 hours, then slowly return to normal activity over the next week.
Many patients stop using opioids within a week. One study found 75% of people no longer needed strong painkillers after the procedure. That’s huge-not just for comfort, but for avoiding addiction and side effects like constipation, drowsiness, and confusion.
You’ll still need to treat the root cause: osteoporosis. Without it, you’re at risk for more fractures. Your doctor will likely prescribe calcium, vitamin D, and medications like bisphosphonates or denosumab to strengthen your bones long-term.
The Bigger Picture: Why These Procedures Are Growing
Over 100,000 of these procedures are done in the U.S. every year. The global market is expected to hit $2.17 billion by 2029. Why? Because the population is aging. One in four women over 50 will have a spinal fracture from osteoporosis. By 2035, that number could rise by 50%.
Recent research even suggests these procedures might save lives. The Vertos II trial found patients who got kyphoplasty or vertebroplasty within two weeks of their fracture had a 28% lower risk of dying within a year compared to those who just rested and took meds. That’s not just about pain-it’s about staying active, avoiding bedsores, pneumonia, and blood clots that come with long-term immobility.
What’s Next?
Newer bone cements made from calcium phosphate are being tested. They’re closer to real bone, harden slower, and produce less heat during curing-reducing the risk of tissue damage. Medtronic’s latest balloon system got FDA approval in March 2023.
But the biggest question still out there? Does restoring height in kyphoplasty actually improve long-term function? The COAST trial, expected to finish in late 2024, will compare mobility, balance, and quality of life between the two procedures over two years. Until then, the choice comes down to your fracture, your goals, and your doctor’s experience.
Final Thoughts
Kyphoplasty and vertebroplasty aren’t magic. They don’t cure osteoporosis. They don’t make your bones strong again. But they do something powerful: they turn unbearable pain into manageable discomfort, and immobility into movement. For many, that’s enough.
If you’re considering one of these procedures, ask your doctor: Is my fracture recent? Is there height loss? What’s my risk for cement leakage? Do I need the extra cost of kyphoplasty-or will vertebroplasty do the job?
The goal isn’t to pick the fanciest option. It’s to pick the one that matches your body, your life, and your needs.
Are kyphoplasty and vertebroplasty the same thing?
No. Both use bone cement to stabilize fractured vertebrae, but kyphoplasty includes an extra step: inflating a balloon inside the bone to restore height before injecting cement. Vertebroplasty injects cement directly without balloon inflation. Kyphoplasty aims to correct deformity; vertebroplasty focuses on pain relief.
Which procedure has less risk of cement leakage?
Kyphoplasty has a lower risk. Cement leaks occur in 9-33% of kyphoplasty cases versus 27-68% in vertebroplasty. The balloon in kyphoplasty creates a controlled space, reducing pressure and the chance cement escapes into surrounding tissues.
Do these procedures cure osteoporosis?
No. They treat the fracture, not the underlying bone weakness. Without managing osteoporosis with medication, calcium, vitamin D, and lifestyle changes, you’re at high risk for more fractures. These procedures are a fix, not a cure.
How soon can I walk after the procedure?
Most patients walk within hours after the procedure, once the sedation wears off. You’ll be monitored for 4-6 hours, then discharged the same day. Light activity is encouraged, but heavy lifting and twisting should be avoided for at least 24 hours.
Is kyphoplasty worth the extra cost?
It depends. If you have significant height loss or spinal deformity, kyphoplasty may help restore posture and reduce future stress on nearby bones. But if your fracture is stable and your main goal is pain relief, vertebroplasty works just as well and costs 20-30% less. Many experts say vertebroplasty offers better value for most patients.
Can these procedures prevent future fractures?
Not directly. In fact, treating one fracture can sometimes increase stress on nearby vertebrae, raising the risk of new ones. The key to preventing future fractures is treating osteoporosis aggressively with medication, diet, and exercise after the procedure.
How long does the pain relief last?
For most people, pain relief is long-lasting-often permanent for that specific fracture. The cement stabilizes the bone, so it no longer moves and causes pain. However, new fractures in other vertebrae can occur, which will cause new pain. That’s why managing osteoporosis is critical.
Are these procedures covered by insurance?
Yes. Medicare and most private insurers cover both kyphoplasty and vertebroplasty if you’ve tried at least 4-6 weeks of conservative treatments like pain meds, bracing, or physical therapy without improvement. Approval rates are over 95% when documentation is complete.
Rachael Gallagher
November 25, 2025 AT 04:18steven patiño palacio
November 25, 2025 AT 12:46Natashia Luu
November 26, 2025 AT 11:33Vineeta Puri
November 28, 2025 AT 02:31Victoria Stanley
November 30, 2025 AT 01:34Andy Louis-Charles
November 30, 2025 AT 02:48Douglas cardoza
November 30, 2025 AT 09:19Adam Hainsfurther
December 2, 2025 AT 03:03stephanie Hill
December 2, 2025 AT 14:20Akash Chopda
December 2, 2025 AT 16:42Nikki C
December 4, 2025 AT 10:50