When a migraine hits, speed and safety matter. You don’t just want relief-you want relief without risking your heart, your focus, or your ability to drive home. Three classes of acute migraine meds-triptans, gepants, and ditans-offer different trade-offs. Understanding their safety profiles isn’t just academic; it can mean the difference between getting back to your day and ending up in the ER.
Triptans: Fast, Effective, But Not for Everyone
Triptans like sumatriptan, rizatriptan, and almotriptan have been the go-to for decades. They work fast-often cutting pain in half within an hour. That’s why they’re still used in over 60% of acute migraine cases. But their mechanism comes with a cost.
Triptans activate serotonin receptors that narrow blood vessels. That’s helpful for migraine, but dangerous if you have heart disease, uncontrolled high blood pressure, or a history of stroke. The American Academy of Family Physicians explicitly warns against using them in these patients. Even if you’re otherwise healthy, you might feel it: chest tightness, flushing, dizziness, or tingling in your hands and face. About 3-8% of users report that crushing chest pressure, and many never take it again after the first dose.
Some side effects are just annoying. Subcutaneous injections cause pain at the site in 40% of users. Nasal sprays leave a bitter aftertaste for a quarter of people. Fatigue and drowsiness are common too. But here’s something important: not every symptom you feel after taking a triptan is caused by the drug. Sometimes, it’s just the migraine itself acting up-like brain fog or weakness. That’s why doctors look at patterns over time, not just one bad reaction.
Still, the data doesn’t lie. In a 2021 analysis of 46,000+ patients across 64 trials, triptans had a higher rate of side effects than newer options. About 1 in 4 users reported something unpleasant. That’s why many stop taking them-even when they work. The JAMA Network Open study found that 55% to 81% of people discontinue triptans due to side effects or fear of risks.
Gepants: The Quiet Contender With Fewer Risks
Gepants-like ubrogepant (Ubrelvy) and rimegepant (Nurtec ODT)-are the new kids on the block. Approved in late 2019, they block a protein called CGRP, which plays a key role in migraine pain. Unlike triptans, they don’t constrict blood vessels. That makes them safe for people with heart conditions who can’t use triptans.
Side effects? Minimal. Nausea happens in just 4-6% of users. Drowsiness affects only 2-4%. There’s a tiny risk of allergic reaction with rimegepant-about 1 in 1,000. No chest tightness. No tingling. No risk of heart attack or stroke from the drug itself.
But they’re slower. Triptans often work in 30 minutes. Gepants take 60 to 90 minutes. If you need to get back to work fast, that’s a real drawback. Still, they last longer. Rimegepant’s half-life is 10-12 hours, meaning it can prevent a rebound headache better than most triptans, which wear off in 2-14 hours.
Real-world feedback backs this up. On Drugs.com, rimegepant has a 7.1/10 rating from nearly 700 users. One person wrote: “No chest pressure like with triptans, just takes longer to work.” That’s the trade-off: patience for peace of mind.
There’s one catch: drug interactions. Rimegepant shouldn’t be taken with strong CYP3A4 inhibitors like ketoconazole or grapefruit juice. These can spike the drug’s levels in your blood. Always tell your doctor what else you’re taking.
Ditans: Powerful But Paralyzing
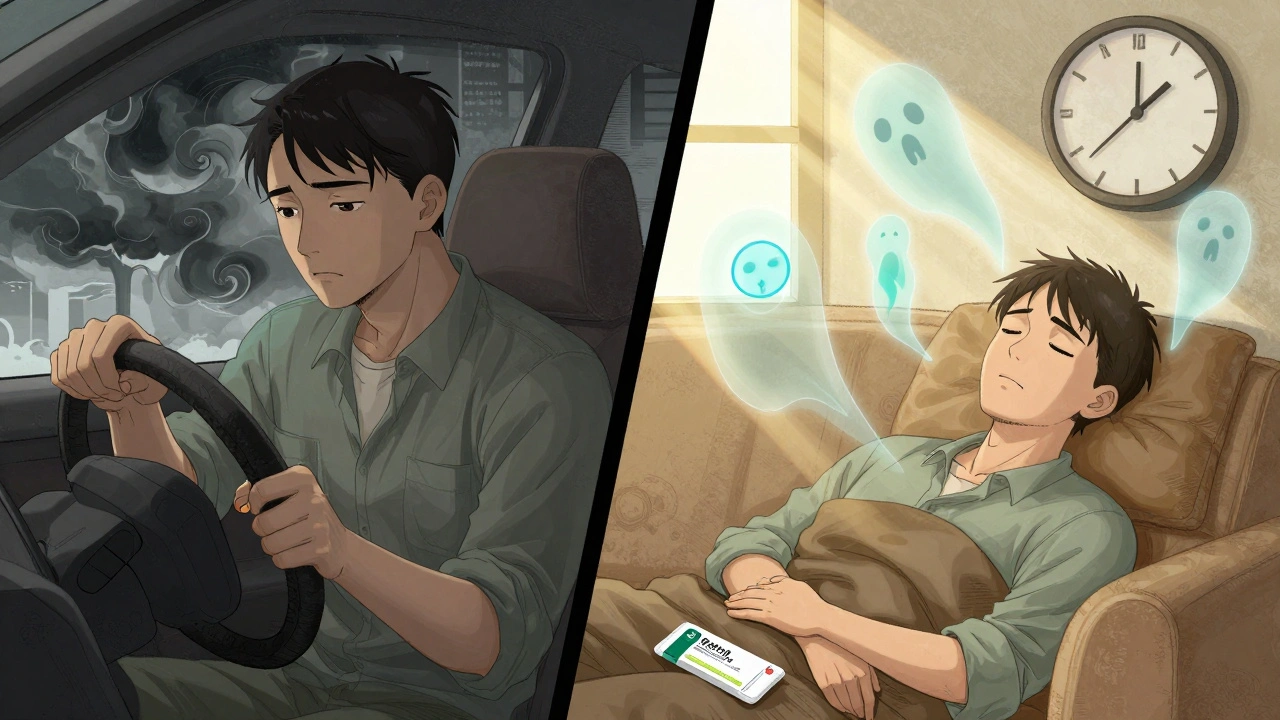
Lasmiditan (Reyvow) is the only ditan on the market. It targets a different serotonin receptor-5-HT1F-so it doesn’t affect blood vessels at all. That means it’s safe for people with heart disease. But it hits your brain hard.
In clinical trials, 18.8% of people taking a standard 100mg dose of lasmiditan felt dizzy. That’s nearly double the placebo rate. Paresthesia (tingling or numbness) hit 9.4%. Sedation? 7.8%. Vertigo? 5.6%. One in three users reported feeling “out of it.”
The FDA requires a black box warning: Do not drive or operate machinery for at least 8 hours after taking Reyvow. A 2021 study showed people were still impaired at the 5-hour mark. That’s not just inconvenient-it’s dangerous. One Reddit user summed it up: “Reyvow made me feel drunk without alcohol.”
It’s not just dizziness. Muscle weakness, fatigue, and cognitive fog are common. In trials, 2.8% of users reported cognitive changes-things like trouble remembering words or focusing. That’s not normal for most migraine sufferers. It’s the drug.
It also carries a theoretical risk for seizures, especially if you’re already on medications that lower your seizure threshold. The Medical Letter advises avoiding it in people with epilepsy or a history of seizures, even though direct evidence is limited.
With an average rating of 5.8/10 on Drugs.com and 63% of negative reviews citing dizziness or sedation, it’s clear: ditans are not for everyone. They’re reserved for patients who can’t use triptans and need something faster than gepants-but only if they can afford to be out of commission for half a day.
Comparing Safety: A Quick Snapshot
| Medication Class | Cardiovascular Risk | Common Side Effects | Onset of Action | Best For |
|---|---|---|---|---|
| Triptans | High-contraindicated in heart disease | Chest tightness, tingling, dizziness, fatigue | 30-60 minutes | Healthy patients needing fast relief |
| Gepants | Very low-safe for heart patients | Nausea (4-6%), drowsiness (2-4%) | 60-90 minutes | Patients with cardiovascular risks or long-term use |
| Ditans | None | Dizziness (18.8%), sedation (7.8%), cognitive fog | 60-90 minutes | Heart patients who can afford to be sedated for 8+ hours |
The numbers tell a clear story. Ditans have the highest overall risk of side effects-almost 3 times more than placebo. Triptans are next. Gepants? Lowest risk by far. But speed and effectiveness matter too. Triptans still win in pain relief at the 2-hour mark. Gepants catch up by 24 hours. Ditans? They relieve pain, but you might not remember how.
What Doctors Really Think
Dr. Elizabeth Loder from Harvard says: “Based on my clinical experience, I don’t think any of these drugs would do a lot better than the triptans” for overall benefit. That’s not because triptans are perfect. It’s because they’re reliable. When they work, they work fast. And for many, that’s worth the risk.
But for others? Not even close. Dr. Rami Burstein points out that lasmiditan’s sedation makes it a poor choice for anyone who needs to function after taking it-parents, drivers, office workers. “It’s not a rescue drug,” he says. “It’s a retreat drug.”
That’s why guidelines are shifting. The American Headache Society now recommends gepants over triptans for patients with cardiovascular risks. It’s not about being trendy-it’s about matching the tool to the person.

Real-Life Decisions
If you’re young, healthy, and your migraines hit like a freight train? Triptans might still be your best bet. Just know the signs of trouble: chest pain, jaw tightness, sudden shortness of breath. Stop the drug and call your doctor.
If you have high blood pressure, angina, or a history of stroke? Skip triptans. Gepants are your safest bet. They’re not perfect, but they’re the closest thing to a clean slate.
If you’ve tried both and still get debilitating migraines? Lasmiditan might be an option-but only if you can plan for a full day off. No driving. No childcare. No work. Just rest.
And if you’re unsure? Talk to your neurologist. Bring your symptom log. Ask: “Which of these has the lowest risk for me?” Because safety isn’t one-size-fits-all.
What’s Coming Next
Zavegepant, a new intranasal gepant, just finished phase 3 trials with a safety profile similar to oral gepants-no vasoconstriction, minimal sedation. It could be available soon, giving people another fast-acting, heart-safe option.
Long-term data is still limited. Only rimegepant has 2-year safety data. The rest? We’re watching. The FDA’s adverse event reports show fewer issues with gepants than triptans, but we need more years.
For now, the choice is clear: know your body, know your risks, and match the drug to your life-not the other way around.
Are triptans safe if I have high blood pressure?
No. Triptans cause blood vessels to narrow, which can raise blood pressure and trigger heart problems. If you have uncontrolled hypertension, heart disease, or a history of stroke, you should avoid them. Gepants are the safer alternative.
Can I drive after taking lasmiditan?
No. The FDA requires you to avoid driving, operating machinery, or doing anything requiring full alertness for at least 8 hours after taking lasmiditan. Many people feel drowsy, dizzy, or mentally foggy for that long-even if they feel fine.
Do gepants cause weight gain or liver damage?
No. Unlike some older migraine preventives, gepants have not been linked to weight gain or liver damage in clinical trials. The most common side effects are mild nausea and drowsiness. Long-term safety beyond 2 years is still being studied, but no major red flags have emerged.
Why are gepants more expensive than triptans?
Gepants are newer and still under patent protection, so they cost more upfront. But if you’ve had to stop triptans due to side effects or heart risks, the cost may be worth it-especially if you avoid ER visits or missed workdays. Some insurance plans cover them with low copays now.
Can I take a gepant and a triptan together?
No. There’s no proven benefit, and combining them increases your risk of side effects without clear advantage. Stick to one acute treatment per attack. If one doesn’t work, wait at least 24 hours before trying another class.
Is it safe to use these meds long-term?
Triptans are generally safe for occasional use (under 10 days/month). Overuse can lead to rebound headaches. Gepants like rimegepant are approved for both acute and preventive use up to 18 times per month. Long-term safety beyond 2 years is still being studied, but no major safety issues have emerged so far.
What to Do Next
Write down your migraine pattern: how often they hit, how long they last, what makes them better or worse. Note any side effects you’ve had from past meds. Bring this to your doctor.
Ask: “Which of these three options is safest for my health history?” Don’t settle for the first prescription. Ask about alternatives. Ask about cost. Ask about real-life impact.
Migraine treatment isn’t about finding the best drug. It’s about finding the right drug-for your body, your life, and your future.

Rudy Van den Boogaert
December 2, 2025 AT 08:57Been on rizatriptan for years, and yeah, the chest tightness is real. Felt like an elephant sat on my ribcage the first time. Switched to Nurtec last year and it’s been a game-changer-no panic, no weird tingles, just quiet relief. Took 90 minutes, but I was able to nap through it and woke up pain-free. Worth the wait.
Also, the fact that it’s an ODT? No swallowing pills when you’re nauseous? Genius.
Gareth Storer
December 3, 2025 AT 04:56Oh wow, so now we’re giving people a choice between ‘heart attack risk’ and ‘zombie mode’? Brilliant. Next up: migraine meds that just teleport you to a quiet room for 8 hours. Maybe with a massage and a cup of chamomile tea?
Meanwhile, my doctor still prescribes sumatriptan like it’s 2005. Guess I’ll keep pretending I’m fine after the ‘chest pressure’…
Pavan Kankala
December 3, 2025 AT 09:19They’re all just corporate toys. Triptans? Made by Big Pharma to keep you dependent. Gepants? Same thing, just rebranded with a fancy acronym. Ditans? Designed to make you docile so you don’t complain about your job.
They don’t want you cured. They want you medicated. The real solution? Fasting, cold showers, and quitting screens. But no one wants to hear that because it doesn’t come in a pill bottle with a $200 copay.
Also, did you know the FDA’s adverse event reports are manually edited? Ask your pharmacist. They’ll laugh.
Martyn Stuart
December 4, 2025 AT 19:59Important note: Gepants are not just ‘safer’-they’re the only option for patients with vascular comorbidities, and that’s not a minor detail. Also, rimegepant is now FDA-approved for preventive use up to 18 times/month, which is huge for chronic migraine sufferers. That’s not just acute relief-it’s disease modification.
And yes, the 60–90 minute onset is a real trade-off, but if you’re not driving, working, or parenting during the attack, it’s manageable. Many patients report better sleep quality after switching-because they’re not terrified of side effects.
Also: grapefruit juice + rimegepant = bad. Don’t be that guy.
Jessica Baydowicz
December 5, 2025 AT 21:21OMG I just switched to Nurtec and I’m crying happy tears 😭
No more ‘am I having a heart attack or is this the med?’ panic. No more lying on the bathroom floor waiting for the dizziness to pass. I can actually read a book after taking it now. My kids didn’t even notice I was gone for two hours. I’m back to being a human.
Also, the minty ODT tastes like a grown-up breath mint. Small wins, people.
Ollie Newland
December 7, 2025 AT 05:19Triptans are still the gold standard for efficacy-no argument there. But the safety profile? Janky. I’ve seen patients with controlled hypertension get chest tightness on sumatriptan, even with normal BP. That’s not anxiety-it’s pharmacology.
Gepants are the quiet revolution. No vasoconstriction, no ER visits, no ‘I thought I was dying’ moments. The lag time? Annoying, sure. But if you’re not in a meeting or driving, it’s a fair exchange.
Ditans? Don’t take them unless you’ve got a sabbatical. I’ve had patients show up to work 6 hours later still blinking slowly like they’re in a fog machine.
Rebecca Braatz
December 8, 2025 AT 21:50If you’re on a triptan and you’ve ever felt ‘off’ after taking it-STOP. Don’t rationalize it. Don’t tell yourself ‘it’s just the migraine.’ That chest pressure? That’s your body screaming. Your neurologist doesn’t know your life. You do.
Try gepants. They’re not magic, but they’re kinder. And if you’re a parent, a driver, or someone who can’t afford to be out of commission for half a day? You deserve better than Reyvow.
You’re not weak for needing a safer option. You’re smart.
Michael Feldstein
December 10, 2025 AT 13:09Has anyone tried combining gepants with non-pharm stuff? I started doing vagal nerve stimulation with a handheld device right before taking Nurtec. Noticed the onset was faster-like 45 minutes instead of 75. Could be placebo, but my headache diary says otherwise.
Also, hydration. I swear, if I drink 16oz of water before the attack hits, the gepant works better. Weird, right?
jagdish kumar
December 10, 2025 AT 19:21Triptans are the opium of the masses.
We’ve been conditioned to believe speed equals healing.
But pain is a messenger.
Maybe we should listen… instead of silencing it with chemicals.
Benjamin Sedler
December 11, 2025 AT 16:46Wait, so you’re telling me the drug that causes chest tightness is still the #1 choice? And the one that makes you feel like you’re drunk without alcohol is the ‘last resort’?
Who designed this system? A committee of sleep-deprived neurologists on Adderall?
Also, I’ve taken Reyvow and I’m 100% certain it’s just a government mind-control experiment. I felt my thoughts get… slower. Like someone pulled the plug on my brain’s Wi-Fi.
zac grant
December 12, 2025 AT 05:58Real talk: Gepants are the unsung heroes. I’ve been on rimegepant for 18 months now. No side effects. No ER trips. No ‘did I just have a mini-stroke?’ panic.
And yes, it’s slower. But I’ve learned to plan. Take it as soon as the aura hits. Sit down. Put on a podcast. Let it work. It’s not a sprint-it’s a slow burn.
Also, insurance finally started covering it after I appealed. Worth the 3 phone calls.
michael booth
December 12, 2025 AT 08:10Heidi Thomas
December 14, 2025 AT 04:10Alex Piddington
December 15, 2025 AT 20:12Just wanted to say: if you’re reading this and you’re scared to ask your doctor about alternatives-you’re not alone. I used to be terrified to say ‘this isn’t working’ or ‘I’m scared of the side effects.’
But your neurologist is there to help you-not judge you.
Bring this post. Print the table. Say: ‘I want to know what’s safest for ME.’
You deserve relief without sacrifice. 💪