Penicillin Allergy Checker
Check if your reaction was a true allergy or side effect
This tool helps you determine if your past reaction to penicillin was likely a true allergy or a common side effect based on timing and symptoms.
Results
More than 10% of people in the U.S. say they’re allergic to penicillin. But here’s the surprising part: less than 1% actually are. That means millions of people are avoiding a safe, effective, and cheap antibiotic because they were misdiagnosed - often as kids, after a harmless rash or stomach upset. And that mistake is costing lives, money, and increasing the risk of dangerous superbugs.
What’s Really Going On When You Say You’re Allergic to Penicillin?
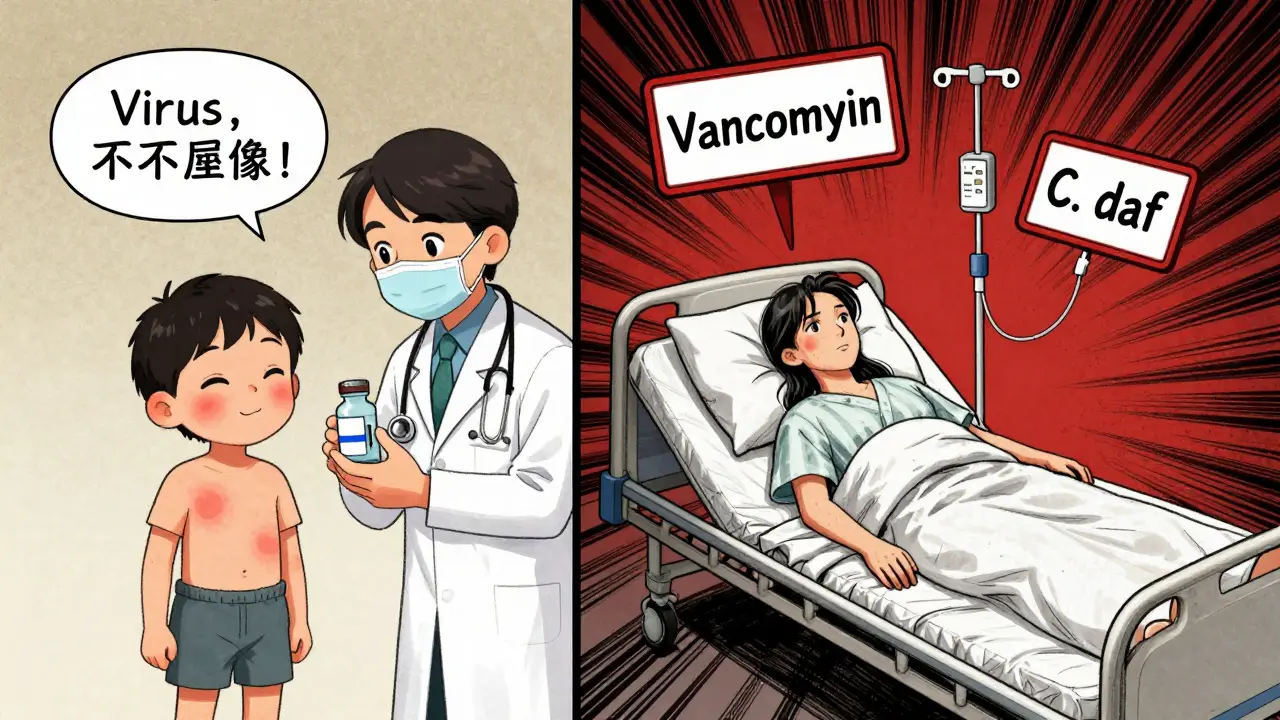
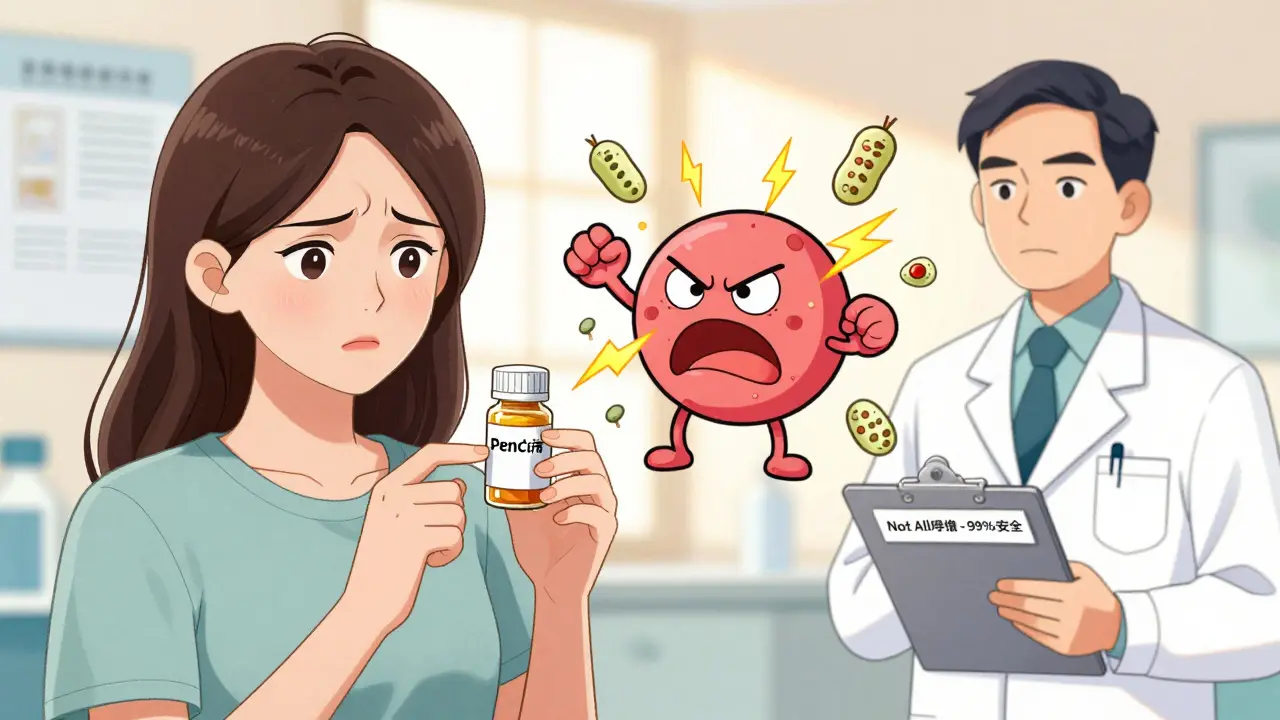
People often confuse side effects with true allergies. If you got a rash after taking penicillin as a child, you might have been told, "You’re allergic." But that rash? It could’ve been from the virus you were fighting - not the antibiotic. Or maybe you had nausea or diarrhea. Those aren’t allergies. They’re common side effects. A true penicillin allergy is an immune system reaction. Your body mistakes the drug for a threat and launches an attack. That’s what causes hives, swelling, trouble breathing, or anaphylaxis - a life-threatening drop in blood pressure. These reactions usually happen within minutes to an hour after taking the drug. But here’s the catch: most people who think they’re allergic never had one. A 2019 study in the Journal of Allergy and Clinical Immunology found that patients with a label of penicillin allergy had 6 more deaths per 1,000 in the year after hospitalization than those without the label. Why? Because doctors avoid penicillin and reach for stronger, riskier antibiotics instead.Side Effects: The Common, Not-So-Scary Reactions
Penicillin can cause unpleasant but harmless reactions. These are side effects - not allergies. They’re predictable, not immune-driven. Think of them like the headache you get from caffeine or the upset stomach from spicy food. Common side effects include:- Mild nausea (affects 5-10% of users)
- Diarrhea (1-2% of users)
- Vaginal yeast infections
- Headache or mild stomach cramps
True Allergies: The Immune System’s Overreaction
True penicillin allergies are rare - but serious. They fall into two categories: immediate and delayed. Immediate reactions (IgE-mediated) happen fast - within minutes to an hour. Symptoms include:- Hives (raised, itchy red welts)
- Swelling of the lips, tongue, or throat
- Wheezing or trouble breathing
- Dizziness or fainting
- Anaphylaxis (a full-body shock reaction)
- Maculopapular rash (flat, red spots that spread)
- Fever
- Joint pain
- Swollen lymph nodes
Why Mislabeling Penicillin Allergy Is Dangerous
When you’re labeled allergic, doctors can’t use penicillin - even if it’s the best choice. So they turn to alternatives like vancomycin, clindamycin, or fluoroquinolones. These drugs are broader-spectrum, more expensive, and more likely to cause serious problems. Here’s what happens:- You’re 70% more likely to get a different antibiotic
- You’re 45% more likely to get one that causes C. diff infection - a severe, sometimes deadly diarrhea
- Costs go up by $463 per hospital stay
- Length of stay increases by half a day on average
How to Find Out If You’re Really Allergic
The good news? You can find out - safely - if you’re truly allergic. There’s a proven, reliable process:- Talk to your doctor - describe your reaction. When did it happen? What were the symptoms? Did you need epinephrine? Did it happen within an hour?
- Get skin tested - an allergist will use tiny amounts of penicillin (PPL and MDM) to prick or inject your skin. If you’re truly allergic, you’ll get a raised bump. This test is 95% accurate.
- Take a supervised dose - if skin testing is negative, you’ll be given a small dose of amoxicillin (a penicillin-type drug) under observation. If nothing happens, you’re not allergic.
What If You Had a Reaction 20 Years Ago?
Here’s something most people don’t know: penicillin allergies fade over time. If you had a reaction as a child, you likely don’t have one now. A 2010 study in the Annals of Allergy, Asthma & Immunology found that 80% of people lose their penicillin allergy after 10 years. After 20 years? The number is even higher. That means if you were told you were allergic in 2005, you’re probably not anymore. But you’re still avoiding penicillin - and paying the price in worse outcomes and higher costs.Who Should Get Tested?
You should consider testing if:- You were labeled allergic as a child
- Your reaction was a rash (not breathing trouble)
- You’ve never had a reaction since
- You’ve been prescribed a different antibiotic because of the label
- You’re planning surgery or have a chronic infection that needs strong antibiotics

Barriers to Testing - And How to Overcome Them
The biggest problem? Access. Many people can’t find an allergist. Insurance doesn’t always cover it. Some doctors don’t know the guidelines. Here’s what’s changing:- Pharmacist-led programs are now common in hospitals. At Kaiser Permanente, they test 15-20 patients a week with a 92% success rate.
- Electronic health records like Epic now include built-in tools to flag patients who might be mislabeled and suggest testing.
- CMS reimbursement for skin testing went up 37% in 2023, making it more attractive for clinics to offer.
- Mobile apps like the CDC’s Penicillin Allergy Assessment Tool (PAAT) help primary care doctors decide who needs referral - with 94% accuracy.
What This Means for You
If you’ve been told you’re allergic to penicillin, don’t assume it’s true. Ask: What exactly happened? Was it a rash? Did I have trouble breathing? Did I need epinephrine? If you’re not sure - or if your reaction was mild - consider getting tested. It’s safe. It’s quick. And it could change your future medical care for the better. You might end up saving money. Avoiding dangerous infections. And even saving your life - by letting your doctor use the best, safest antibiotic for your condition.Frequently Asked Questions
Can you outgrow a penicillin allergy?
Yes. Studies show that about 80% of people who had a penicillin allergy as a child lose it after 10 years. The immune system stops recognizing the drug as a threat. If you were labeled allergic years ago and haven’t had a reaction since, you’re likely no longer allergic - but you won’t know for sure without testing.
Is a rash always a sign of penicillin allergy?
No. A rash that appears days after starting penicillin - especially if you were sick with a virus like mono or the flu - is often not an allergy. It’s a common reaction to the infection, not the drug. True allergic rashes (hives) appear within minutes to hours and are raised, itchy, and move around the body. A flat, red, spreading rash is rarely IgE-mediated.
What’s the difference between a side effect and an allergic reaction?
Side effects are predictable, non-immune responses like nausea or diarrhea - they happen to many people and aren’t dangerous. Allergic reactions involve your immune system attacking the drug, causing symptoms like hives, swelling, breathing trouble, or anaphylaxis. Only immune reactions are true allergies.
Can I take other antibiotics if I’m allergic to penicillin?
Yes - but only if you’re truly allergic. Many people avoid all penicillin-family drugs (like amoxicillin or ampicillin) unnecessarily. If you’re not truly allergic, you can safely take them. Even if you are allergic, many other antibiotics (like cephalosporins) are still safe for most people. Don’t assume all antibiotics are off-limits.
Is penicillin skin testing safe?
Yes. Skin testing uses tiny amounts of penicillin and is done under medical supervision with emergency equipment on hand. In large studies involving tens of thousands of patients, serious reactions during testing are extremely rare - and almost never occur during the oral challenge phase if skin testing is negative.
Adarsh Dubey
December 24, 2025 AT 04:48Interesting breakdown. I always assumed my childhood rash meant I was allergic, but now I realize it was probably just a virus. Glad to see the data backs this up.
Bartholomew Henry Allen
December 25, 2025 AT 22:31Unacceptable that so many are misdiagnosed. This is a systemic failure in American healthcare. We need mandatory reevaluation protocols for all penicillin labels.
claire davies
December 27, 2025 AT 19:30Oh my goodness, I had no idea! I was told I was allergic after a silly rash at 7 - and now I’m 42 and have been avoiding penicillin for decades. I just got chills reading that 80% lose the allergy after 10 years. I’m booking an allergist appointment tomorrow. 🙌 Thank you for this eye-opening piece - it’s the kind of info that could literally save lives, not to mention spare us from those gross, expensive alternatives that leave you feeling like a zombie.
Chris Buchanan
December 28, 2025 AT 05:02So let me get this straight - millions of people are walking around with a fake allergy label because someone in 1998 saw a rash and said ‘nah, don’t take this again’? And now we’re stuck with antibiotics that cost more and cause C. diff? Bro. We’re literally fighting superbugs with our own ignorance. This isn’t just a medical issue - it’s a national comedy of errors.
Raja P
December 29, 2025 AT 20:28My mom got labeled allergic after a rash as a kid. She never got tested. Now she’s got a UTI and they’re giving her something that made her super dizzy. I’m gonna push her to get tested. Feels wrong to avoid something so safe.
Joseph Manuel
December 31, 2025 AT 18:33The statistical implications of this mislabeling are profound. The CDC’s $20 billion cost estimate is underinclusive - it fails to account for long-term resistance development and downstream morbidity. A meta-analysis of 17 cohort studies confirms a 2.3-fold increase in treatment failure rates among mislabeled patients.
Andy Grace
January 1, 2026 AT 20:23I’ve seen this in my practice. Patients come in terrified of penicillin, but when you ask them what happened - it’s just a rash after a cold. They’ve been avoiding it for 15 years. It’s tragic. I wish more doctors would push for testing.
Abby Polhill
January 2, 2026 AT 11:00Penicillin allergy mislabeling is a classic case of diagnostic inertia. The IgE-mediated response is often conflated with non-IgE-mediated reactions - particularly maculopapular rashes associated with viral prodromes. This leads to inappropriate antibiotic stewardship and increased beta-lactam avoidance, which correlates with higher rates of MRSA colonization and VRE acquisition.
Lindsey Kidd
January 3, 2026 AT 12:27OMG I’m so doing this!! 🙏 I thought I was allergic since I got a rash at 8… turns out I just had mono. I’m booking my skin test today. My doctor never even mentioned testing! 😅 #PenicillinFreedom
Austin LeBlanc
January 3, 2026 AT 13:05Wow, so you’re telling me I’ve been avoiding penicillin for 20 years because my mom panicked over a rash? And now I’m paying for it with worse antibiotics? This is the dumbest thing I’ve ever heard. Why isn’t this all over the news? People are dying because of lazy doctors and overcautious parents.
niharika hardikar
January 4, 2026 AT 10:19It is imperative that patients be educated regarding the clinical distinction between adverse drug reactions and true immunoglobulin E-mediated hypersensitivity. The proliferation of unverified allergy labels constitutes a public health hazard, and primary care providers bear responsibility for failing to refer patients for formal allergological evaluation.
Rachel Cericola
January 4, 2026 AT 23:19I’m an infectious disease pharmacist and I’ve led over 200 penicillin de-labeling programs. The data is rock solid - 99% of people who get tested are fine. I’ve seen people cry because they finally realized they could’ve taken amoxicillin for their ear infections instead of being stuck with clindamycin that gave them C. diff. This isn’t just about antibiotics - it’s about trust in medicine. We’ve scared people into avoiding the safest option. Let’s fix that. If you think you’re allergic - get tested. It’s 1.5 hours. No needles, no pain, no risk. And it could change your life.
Blow Job
January 5, 2026 AT 01:36My cousin got tested last year. Turned out she wasn’t allergic. She’s been on penicillin for every infection since - no issues. She said it felt like being unchained. Seriously, if you think you’re allergic, don’t just assume. Get checked. It’s easy, safe, and way cheaper than all those other antibiotics.
Christine Détraz
January 5, 2026 AT 14:14My dad was told he was allergic in the 70s after a rash. He never questioned it. Last year he got pneumonia. They gave him azithromycin - he got super dizzy and spent three days in the hospital. Turns out penicillin would’ve been perfect. We’re getting him tested next month. I’m just glad we found this info before something worse happened.