Drug Side Effect Type Checker
Check if a medication's side effects are predictable or unpredictable based on pharmacology research. This tool helps you understand the difference between expected dose-dependent reactions and rare, unpredictable immune-mediated reactions.
Enter a drug name and click "Check Side Effect Type" to see results.
When you take a pill, you expect it to help - not hurt. But sometimes, medications cause problems. Not all side effects are the same. Some you can see coming. Others strike out of nowhere. Understanding the difference between predictable and unpredictable side effects isn’t just academic - it’s life-saving.
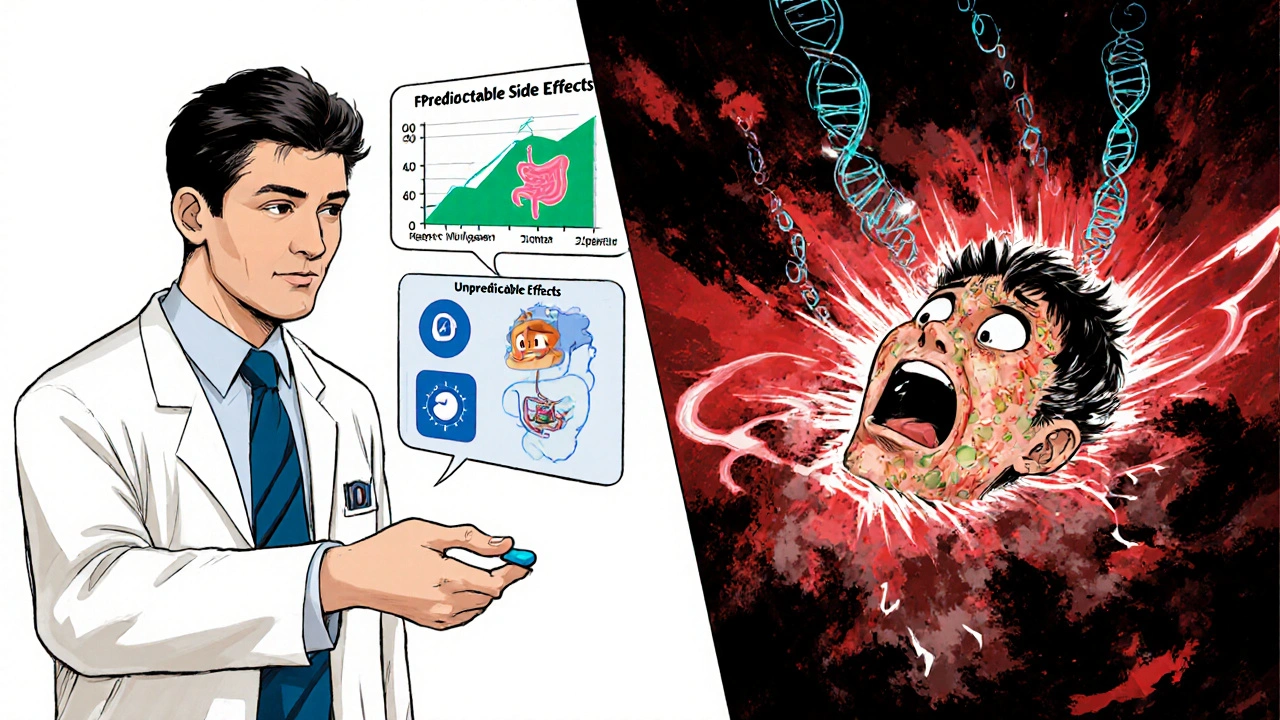
Predictable Side Effects: The Expected Risks
Predictable side effects, also called Type A reactions, make up 75-80% of all adverse drug reactions. These aren’t accidents. They’re direct extensions of how the drug works. If a medication lowers blood pressure, it’s no surprise if someone feels dizzy. If it reduces stomach acid, it might cause diarrhea. These reactions follow the rules of pharmacology. They’re dose-dependent. Take more, get more side effects. Take less, and they fade. Common examples include stomach bleeding from NSAIDs like ibuprofen or naproxen. These drugs block enzymes that protect the stomach lining. At normal doses, the risk is low - about 1-2%. But crank up the dose, and that risk jumps to 10-15%. That’s not random. That’s chemistry. Another classic is low blood sugar from metformin in people with kidney issues. The drug works by reducing liver glucose output. If the kidneys can’t clear it properly, levels build up - and blood sugar plummets. The good news? These reactions are usually reversible. Stop the drug, lower the dose, or give supportive care, and things get better. Mortality is low. Most are managed in outpatient settings. Doctors expect them. Guidelines tell them to monitor kidney function, liver enzymes, or blood counts. They’re the low-hanging fruit of drug safety.Unpredictable Side Effects: The Silent Threats
Then there are the unpredictable ones - Type B reactions. These make up only 20-25% of side effects, but they’re responsible for nearly 20% of serious hospitalizations. And they’re terrifying because they make no sense. A healthy 24-year-old takes a single dose of sulfamethoxazole - a common antibiotic - and wakes up with 30% of their skin peeling off. That’s toxic epidermal necrolysis. No overdose. No prior reaction. No warning. Just a deadly immune response triggered by a drug that should’ve been harmless. These reactions aren’t about dose. They’re about who you are. Genetics. Immune quirks. Unknown biological switches. One person gets anaphylaxis from penicillin. Another takes the same drug and feels fine. Why? In some populations, carrying the HLA-B*1502 gene makes you 100 times more likely to develop Stevens-Johnson syndrome from carbamazepine. That’s not a side effect - it’s a genetic landmine. Other examples include hemolytic anemia in people with G6PD deficiency after taking sulfa drugs or aspirin. Or anaphylaxis from vancomycin - not because of allergy, but because the drug directly triggers mast cells to release histamine. These are called pseudoallergic reactions. They look like allergies but aren’t. And they’re impossible to predict without testing.Why the Difference Matters in Real Life
The distinction isn’t just textbook material. It changes how doctors treat patients. For predictable reactions, the strategy is simple: monitor, adjust, educate. If you’re on an NSAID, your doctor checks your kidney function. If you’re on warfarin, they track your INR. If you’re on metformin and you’re over 70, they lower the dose. These are standard precautions. They work. For unpredictable reactions, it’s different. You can’t monitor your way out of it. You need to know who’s at risk before giving the drug. That’s where genetic testing comes in. Before prescribing abacavir for HIV, doctors test for HLA-B*5701. If it’s positive, they don’t give the drug. Period. This single test cut abacavir-related hypersensitivity from 5% to under 0.5%. But here’s the problem: we only have genetic tests for a few of these reactions. Right now, we can screen for maybe 30% of high-risk Type B reactions. That means 70% still come out of nowhere. A patient on acetaminophen - the safest painkiller - develops Stevens-Johnson syndrome. No known risk factors. No family history. No genetic marker. Just bad luck. That’s what keeps doctors up at night.
The Hidden Costs and System Gaps
The U.S. spends $30.1 billion a year managing drug side effects. Of that, $22.6 billion goes to predictable reactions - because they’re so common. Even though they’re less deadly, they happen to millions. A few extra ER visits, a few days in the hospital, a few prescriptions for stomach protectants - it adds up fast. Unpredictable reactions cost less overall - $7.5 billion - but each case is expensive. A single case of toxic epidermal necrolysis can cost over $100,000 in ICU care. Many require skin grafts, long-term rehab, or result in death. And because they’re rare, hospitals aren’t always prepared. Emergency rooms don’t have protocols for every possible genetic reaction. That’s why only 42% of serious side effects are correctly classified when first reported. The FDA has 64 active Risk Evaluation and Mitigation Strategies (REMS) programs - mostly for drugs with unpredictable risks. These require special training, patient registries, or restricted distribution. It’s not just about safety. It’s about legal protection for drug makers and liability control for hospitals.What’s Changing - and What’s Not
Technology is helping. In 2023, the FDA approved the first AI-powered tool to help doctors adjust warfarin doses based on a patient’s CYP2C9 and VKORC1 genes. That’s a win for predictable reactions. It reduces bleeding risk by 30%. For unpredictable reactions, progress is slower. The NIH’s All of Us program has found 17 new gene-drug links - including one that connects HLA-B*15:02 with phenytoin-induced skin reactions in non-Asian populations. That’s huge. It means we’re not just looking at Asian patients anymore. We’re expanding our understanding. But artificial intelligence still struggles. Google Health trained an AI on 10 million electronic health records. It predicted Type A reactions with 89% accuracy. For Type B? Only 47%. Why? Because these reactions depend on tiny, unknown interactions between genes, environment, and immune history. We don’t have the data. We don’t even know what to look for.
What You Can Do
If you’re on medication, here’s what matters:- Know your family history. Have relatives had bad reactions to drugs? That’s a red flag.
- Ask your doctor: “Is this drug linked to any rare but serious reactions?”
- If you’re prescribed a drug with known genetic risks (like abacavir, carbamazepine, or allopurinol), ask if testing is available.
- Don’t ignore early warning signs. A rash, fever, or blistering after starting a new drug? Don’t wait. Get checked immediately.
- Keep a list of all your medications - including over-the-counter and supplements. Many reactions happen from interactions, not single drugs.
What the Future Holds
By 2030, the goal is to cut severe unpredictable reactions by half through widespread genetic screening. That’s ambitious. But it’s possible - if we invest in testing, data sharing, and research. Right now, only 38% of U.S. hospitals do any kind of pharmacogenetic testing. That number is growing, but slowly. And even in those hospitals, testing isn’t always done for the right drugs. We’re still playing catch-up. The truth is, we’ll never eliminate unpredictable side effects. They’re built into human biology. But we can reduce them. Not by guessing. Not by hoping. But by knowing - who you are, what your genes say, and what your body can’t tolerate. Drug safety isn’t about eliminating risk. It’s about understanding it. And that starts with knowing the difference between what’s expected - and what’s a surprise.Are all side effects dangerous?
No. Many side effects are mild and temporary - like nausea from antibiotics or drowsiness from antihistamines. These are often predictable and go away as your body adjusts. Dangerous side effects are usually severe, unexpected, or persistent. If you experience skin rash, swelling, trouble breathing, or unexplained bleeding, seek medical help right away.
Can I prevent unpredictable side effects?
Sometimes. For certain drugs, genetic testing can identify high-risk patients before they’re exposed. For example, testing for HLA-B*5701 before giving abacavir prevents a life-threatening reaction. But for most unpredictable reactions, there’s no test yet. The best defense is knowing your medical history, telling your doctor about past reactions, and watching for early symptoms like rash or fever.
Why do some people react badly to drugs others tolerate?
It’s usually genetic. Your genes control how your body breaks down drugs, how your immune system responds, and even how your skin cells react. Small differences - like carrying HLA-B*1502 - can make a drug safe for most people but deadly for you. Environmental factors, like infections or other medications, can also trigger unexpected reactions in vulnerable individuals.
Do natural supplements have side effects too?
Yes. Many people assume herbal products are safe because they’re “natural,” but that’s not true. St. John’s wort can interfere with birth control and antidepressants. Kava can cause liver damage. Goldenseal can raise blood pressure. These reactions are often unpredictable and underreported because supplements aren’t regulated like prescription drugs.
What should I do if I think I had a drug reaction?
Stop the drug and contact your doctor immediately. Don’t wait to see if it gets better. Document what you took, when, and what symptoms you had. If it’s serious - like difficulty breathing, swelling, or skin peeling - go to the ER. You can also report it to your country’s pharmacovigilance system (like the FDA’s MedWatch in the U.S.) to help improve drug safety for others.
Are older adults more at risk for side effects?
Yes. As people age, their kidneys and liver process drugs more slowly. They often take multiple medications, increasing interaction risks. Many side effects in older adults - like confusion, dizziness, or falls - are mistaken for aging, when they’re actually drug reactions. Doctors should always review medications in patients over 65 and consider lower doses.
Nicole Ziegler
November 20, 2025 AT 03:52Ravi boy
November 21, 2025 AT 04:13Bharat Alasandi
November 21, 2025 AT 20:30Aruna Urban Planner
November 22, 2025 AT 04:36Matthew Karrs
November 23, 2025 AT 14:23Shiv Karan Singh
November 24, 2025 AT 15:28Matthew Peters
November 25, 2025 AT 05:03Michael Fessler
November 26, 2025 AT 16:59Liam Strachan
November 27, 2025 AT 21:57Gerald Cheruiyot
November 29, 2025 AT 14:15Summer Joy
November 30, 2025 AT 00:23Kristi Bennardo
December 1, 2025 AT 00:57