When you have chronic kidney disease (CKD), what you eat isn’t just about comfort or preference-it’s a tool to slow down damage and avoid dialysis longer. One of the most important, yet confusing, parts of this is protein. Too much can overload your kidneys. Too little can leave you weak, hungry, and at risk for muscle loss. The right amount? It depends on your stage of kidney disease, your age, your weight, and even what kind of protein you’re eating.
What Protein Does in Kidney Disease
Your kidneys filter waste from your blood. When you eat protein, your body breaks it down into nitrogen-based waste like urea. Healthy kidneys handle this easily. But when kidney function drops, that waste builds up. That’s why cutting protein seems like a logical fix. Less protein = less waste = less strain on your kidneys.
But it’s not that simple. Protein also keeps your muscles strong, helps your immune system work, and supports healing. If you cut too much, you risk protein-energy wasting, a dangerous condition that affects up to half of people with advanced CKD. The goal isn’t to starve yourself of protein-it’s to find the sweet spot that protects your kidneys without starving your body.
Protein Targets by CKD Stage
Not all stages of kidney disease need the same protein rules. The guidelines split this clearly:
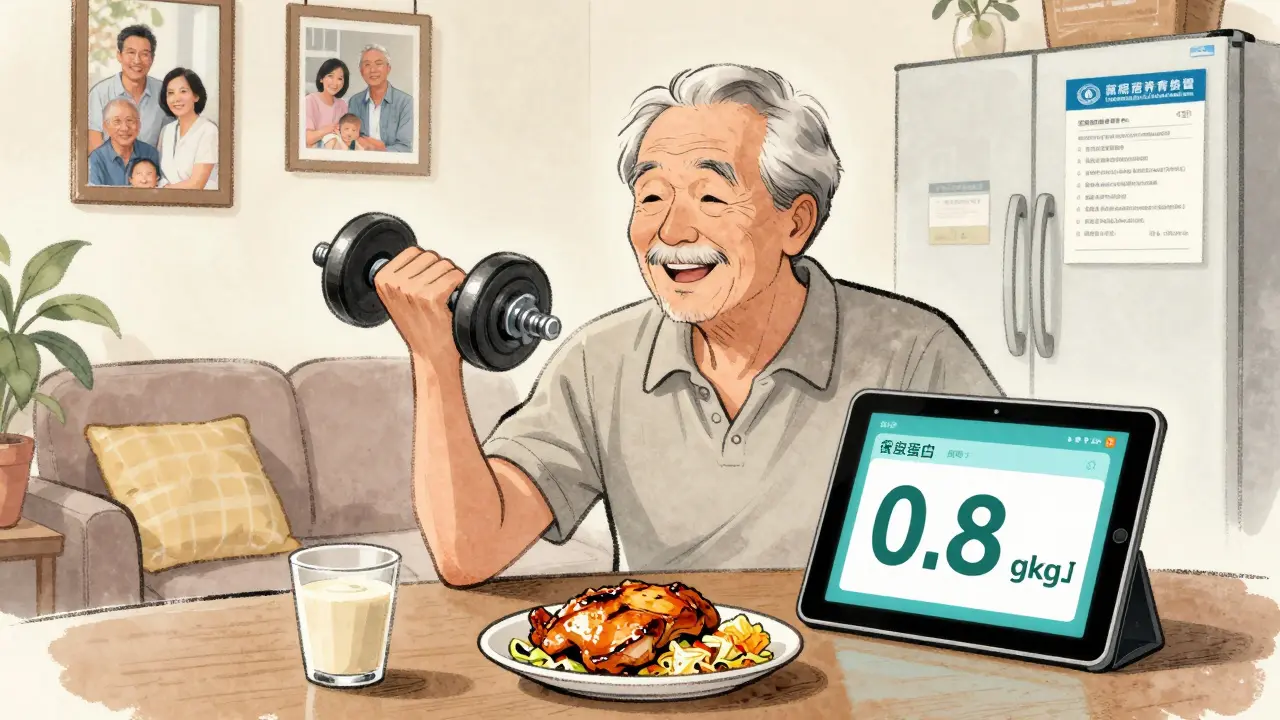
- CKD Stages 1-2 (GFR ≥60): Your kidneys are still working well, but there’s early damage. The recommendation here is no more than 0.8 grams of protein per kilogram of body weight per day. For someone who weighs 150 pounds (68 kg), that’s about 54 grams of protein daily. This isn’t a drastic cut-it’s more about avoiding excess. Studies show that going above 1.3 g/kg/day may speed up kidney decline, even at this early stage.
- CKD Stages 3-4 (GFR 15-59): This is where protein restriction becomes more focused. The standard target is 0.55-0.60 g/kg/day. For a 150-pound person, that’s 40-54 grams daily. Some newer research suggests 0.6-0.8 g/kg/day may be safer, especially for older adults. The key is balance: enough to prevent muscle loss, but low enough to reduce waste buildup.
- CKD Stage 5 (GFR <15, not on dialysis): Protein targets stay in the 0.55-0.60 g/kg/day range, but many patients here are at high risk for malnutrition. Doctors often add keto acid analogues-special supplements that help your body make protein without creating waste. These are prescribed in about 15% of stage 4-5 cases in Europe.
There’s one big exception: if you have diabetes along with CKD, your protein target shifts slightly. The American Diabetes Association recommends 0.8-0.9 g/kg/day to protect your kidneys while keeping your blood sugar stable. Too little protein here can hurt your ability to heal and fight infection.
Animal vs. Plant Protein: What Matters More
Not all protein is created equal-especially for your kidneys.
Animal proteins (meat, eggs, dairy, fish) are called “high-quality” because they contain all the essential amino acids your body can’t make on its own. But they also produce more urea and phosphorus. Red meat, in particular, creates 50% more advanced glycation end products (AGEs) than plant proteins. These compounds trigger inflammation and oxidative stress, which accelerate kidney damage.
Plant proteins (beans, lentils, tofu, nuts, whole grains) are gentler. They produce 20-30% less urea and phosphate per gram. A 2021 meta-analysis found that replacing just 30% of animal protein with plant protein lowered the risk of CKD progression by 14% and cut death risk by 11%. That’s huge.
But here’s the catch: most plant proteins are low in one or two essential amino acids-like lysine or methionine. That means you can’t just swap chicken for lentils and call it a day. You need to combine them. A meal with rice and beans, or hummus with whole wheat pita, gives you a complete amino acid profile. Soy is the only plant protein that naturally has all nine essential amino acids, making it a top choice for CKD diets.
For stage 4-5 patients, plant proteins can be tricky because they’re often high in potassium. Sweet potatoes, spinach, beans-all great for healthy people, but risky if your kidneys can’t flush out potassium. That’s why working with a renal dietitian is critical. They can help you pick low-potassium plant options like cabbage, cauliflower, or apples, and still meet your protein needs.
Who Should Eat More Protein?
Not everyone needs to restrict. Some people actually need more.
Older adults with CKD are a major group. A 2024 JAMA Network Open study found that those over 65 with early-stage CKD who ate more protein (up to 0.8-1.0 g/kg/day) had lower death rates. Why? Because they’re more likely to die from heart disease or infection before their kidneys fail. Muscle loss in older adults speeds up frailty, falls, and hospitalizations. In this group, protecting muscle may matter more than slowing kidney decline.
Same goes for people who are underweight, recovering from surgery, or fighting infection. If you’re losing weight unintentionally or feeling weak all the time, your doctor may adjust your protein target upward-even if you’re in stage 4. The goal isn’t to follow a number blindly. It’s to keep you strong enough to live well.
Real-Life Challenges and How to Beat Them
People who try to follow these guidelines often hit walls.
On patient forums, 74% say they’re constantly hungry after cutting protein. 62% report muscle weakness. 58% feel isolated because they can’t eat with family or friends. One Reddit user wrote: “Cutting from 100g to 45g daily made me feel like I was fading away.”
But here’s the good news: those who work with a renal dietitian have 82% better adherence and report higher quality of life. Why? Because dietitians don’t just give numbers-they give meals.
Successful strategies include:
- Using apps like the National Kidney Foundation’s Protein Target Calculator (downloaded over 47,000 times since 2023) to track daily intake.
- Meal prepping with kidney-friendly recipes from Kidney Kitchen, which gets over 1.2 million visits a month.
- Using MyFitnessPal with a renal database to log protein in mixed dishes-something 87% of patients struggle with.
- Choosing high-biological-value proteins: eggs, milk, chicken, fish, and soy. Half your daily protein should come from these sources.
Many people also benefit from keto acid analogues like Ketosteril. These supplements let your body rebuild protein without producing urea. They’re not magic, but they help when you’re stuck between too little and too much.

Getting the Right Support
Only 35% of nephrologists refer patients to renal dietitians-even though guidelines say they should. That’s a huge gap. You can’t learn this stuff from a blog. It takes time, personalized planning, and ongoing support.
Medicare now covers 3 hours of initial nutrition counseling and 2 hours of follow-up per year for CKD patients. That’s a big step. Use it. Ask your doctor for a referral. Bring your food log. Ask questions like:
- “Is my protein level helping or hurting my kidneys?”
- “Can we adjust this based on how I feel?”
- “What are my best protein sources that won’t spike my potassium or phosphorus?”
The learning curve takes 3-6 months. Don’t expect to get it perfect on day one. But with the right help, you can eat well, feel stronger, and delay dialysis longer.
The Future of Protein in CKD
The field is moving fast. In 2024, the American Society of Nephrology launched personalized protein algorithms using machine learning. These tools look at your genetics, urea levels, and diet patterns to predict how your body responds to protein-not just your weight.
The NIH-funded PRECISE-CKD trial is testing whether tailoring protein targets to your individual urea production works better than the old “grams per kilogram” formula. Early results are promising.
Scientists are also developing new plant-based protein concentrates with reduced potassium. Imagine tofu or lentil flour that gives you all the protein you need without the potassium spike. That could be a game-changer.
One thing’s clear: the future isn’t about one-size-fits-all protein limits. It’s about smart, individualized plans that protect your kidneys while keeping you alive, strong, and able to enjoy your meals.
How much protein should I eat if I have stage 3 CKD?
For stage 3 CKD (GFR 30-59), aim for 0.55-0.60 grams of protein per kilogram of body weight daily. For a 150-pound person, that’s about 40-54 grams. If you’re older, underweight, or have diabetes, your target may be higher-up to 0.8 g/kg. Always check with a renal dietitian to personalize this.
Can I eat plant-based protein with kidney disease?
Yes, and it’s often better for your kidneys. Plant proteins produce less waste and inflammation. But they’re usually low in some essential amino acids. Combine them-like beans with rice or hummus with whole wheat-to get a complete profile. Soy is the best single plant source. Watch potassium levels in foods like spinach and sweet potatoes if you’re in stage 4 or 5.
Does protein restriction really delay dialysis?
Yes. The 2022 Cochrane Review found that keeping protein at 0.6-0.8 g/kg/day reduces the risk of reaching end-stage kidney disease by 31% over 2-4 years compared to unrestricted diets. This can delay dialysis by 6-12 months. But it only works if you stick with it-adherence rates in studies average just 58%.
Why do I feel weak on a low-protein diet?
You may be getting too little protein for your body’s needs. Protein-energy wasting is common in advanced CKD. If you’re losing weight, feeling tired, or losing muscle, your target may be too low. Talk to your doctor or dietitian. You might need more protein, or supplements like keto acid analogues to help your body use protein efficiently without extra waste.
Should I use protein supplements for kidney disease?
General protein powders (whey, casein) are usually not recommended-they add too much waste. But specialized medical foods like keto acid analogues (e.g., Ketosteril) are prescribed for stage 4-5 patients. These provide the building blocks for protein without the nitrogen waste. Only use them under medical supervision.
How do I track protein in mixed meals like pasta or soup?
Use apps like MyFitnessPal with a renal database, or the National Kidney Foundation’s Protein Target Calculator. Many people struggle with this-87% report difficulty. Learn to estimate portions: 1 oz of meat = 7g protein, 1 egg = 6g, ½ cup beans = 7g. Keep a food log for a few days and bring it to your dietitian for help.

Todd Nickel
December 31, 2025 AT 18:19It's wild how much nuance there is in protein intake for CKD. I used to think less was always better until my nephrologist showed me the data on muscle wasting in stage 4. Turns out, going below 0.5 g/kg/day for too long can trigger a cascade-loss of strength, slower wound healing, even increased infection risk. The sweet spot isn't just about numbers, it's about quality too. Plant-based proteins like lentils and tofu produce less uremic toxin load than red meat. I track mine with a food app and adjust based on monthly labs. It's not glamorous, but it keeps me off dialysis longer than most doctors expected.
Also, hydration matters more than people admit. If you're not drinking enough water, even moderate protein can feel like a burden on the kidneys. I aim for 1.5–2L daily unless my sodium’s up. Small stuff, but it adds up.
And yeah, don’t trust random Reddit advice. Talk to a renal dietitian. They’re not just nutritionists-they’re kidney whisperers.
Austin Mac-Anabraba
December 31, 2025 AT 19:09Let’s be honest-this whole protein restriction thing is a placebo-driven illusion created by pharmaceutical-aligned nephrology societies. The real issue? Industrial food systems. You think your 0.6 g/kg is safe? What about the phosphorus binders? The processed ‘renal-friendly’ foods loaded with sodium and artificial additives? They’re not fixing your kidneys-they’re selling you a lifestyle subscription. The only thing that truly slows CKD progression is whole, unprocessed food and fasting. Period. The guidelines are corporate propaganda dressed in medical jargon.
Phoebe McKenzie
December 31, 2025 AT 22:00Wow. Just… wow. You people are still falling for this outdated, outdated, OUTDATED medical dogma? Did you know that the American Kidney Fund gets funding from Big Pharma? They push these ‘protein limits’ so you’ll stay on expensive meds longer. Meanwhile, real healers-functional medicine doctors, naturopaths-they tell you to eat MORE protein if you’re losing muscle. You’re not a broken machine. You’re a living organism that needs nourishment. Stop starving yourself for a number on a chart. Your body knows better than some 1990s study.
gerard najera
January 2, 2026 AT 04:34Protein isn’t the enemy. Mismanagement is.
Stephen Gikuma
January 3, 2026 AT 00:33Who wrote this? Some CDC drone? The real problem isn’t protein-it’s the government letting Chinese imports flood our food supply with heavy metals and glyphosate. That’s what’s wrecking kidneys, not a steak. We need to ban imported soy and beef, rebuild domestic agriculture, and get back to real food. This ‘0.6 g/kg’ nonsense? It’s part of the globalist agenda to make us weak and dependent. Eat meat. Eat eggs. Fight back.
Bobby Collins
January 4, 2026 AT 21:21ok but like… what if you just… eat less protein but like… only organic grass fed beef and no processed stuff? idk i just feel like if its clean its fine? 🤷♀️
Layla Anna
January 6, 2026 AT 04:42Thank you for this post 😊 i’ve been stage 3 for 3 years and this actually made sense for once 🙏 i’ve been scared to eat chicken because i thought it was bad but now i know it’s about the amount not the type! love how you broke it down 🌸
Heather Josey
January 7, 2026 AT 02:10This is an exceptionally clear and clinically grounded summary. For patients navigating CKD, the balance between protein restriction and preservation of lean body mass is one of the most critical yet under-discussed aspects of care. I encourage all individuals with stage 3 or higher CKD to consult with a registered dietitian specializing in renal nutrition. Individualization-not generalization-is the cornerstone of successful dietary management. Thank you for elevating this conversation with evidence-based clarity.
Olukayode Oguntulu
January 7, 2026 AT 07:46Let me reframe this through the lens of biopolitical economy: the protein paradigm in CKD is not a physiological directive but a disciplinary mechanism-standardized, quantified, and commodified by the renal-industrial complex. The 0.6 g/kg recommendation is less a scientific truth than a bureaucratic artifact designed to optimize compliance and pharmacological dependency. One must interrogate not merely the quantity, but the ontology of the ‘diet’ itself. Is nutrition a tool of liberation-or a cage wrapped in kale?
LIZETH DE PACHECO
January 7, 2026 AT 16:35Hey, I’ve been on dialysis for 5 years now and this post made me feel seen. I used to panic about every bite, but now I know I can have a small chicken breast at dinner without feeling guilty. You’re right-it’s not about deprivation. It’s about smart choices. Keep sharing stuff like this. It helps more than you know 💪❤️
Bryan Anderson
January 8, 2026 AT 05:49Interesting breakdown. I’ve been following the 0.6 g/kg guideline for my stage 3 CKD, but I’ve noticed that my energy levels dip if I go below 0.65 for more than a week. I wonder if age and activity level play a bigger role than the guidelines acknowledge. My 72-year-old dad, who walks 3 miles daily, seems to handle 0.75 g/kg fine. Maybe the numbers need a little more personalization.
Matthew Hekmatniaz
January 8, 2026 AT 11:15I appreciate how this post avoids fear-mongering. Too many health articles treat CKD like a death sentence. The truth is, many people live well for years with proper management. What’s missing here, though, is the role of gut health. Emerging research suggests the microbiome influences uremic toxin production. Maybe the type of protein matters less than what you’re eating alongside it-fiber, fermented foods, polyphenols. Worth a look if you’re optimizing long-term.
Dusty Weeks
January 8, 2026 AT 20:06protein is a scam. they just want you to buy renal shakes and pills. eat steak. eat eggs. eat butter. the kidney is a filter not a dictator. #freeprotein
Bill Medley
January 10, 2026 AT 06:01The referenced guidelines are consistent with the 2020 KDIGO Clinical Practice Guideline Update. Adherence to individualized protein intake, particularly in non-dialysis-dependent CKD, remains associated with reduced all-cause mortality and delayed progression to end-stage renal disease. Clinical application requires monitoring of serum albumin, pre-albumin, and mid-arm circumference for early detection of protein-energy wasting.
Richard Thomas
January 11, 2026 AT 10:30There’s a deeper question here that no one’s asking: Why do we treat kidneys like fragile glassware instead of resilient organs? Evolution didn’t design us to live on 0.6 g/kg for decades. We evolved eating whole animals-muscle, organs, bone broth. The real problem isn’t protein-it’s the isolation of nutrients. We’ve forgotten that food is a system, not a spreadsheet. Maybe the answer isn’t less protein… but more collagen, more glycine, more bone broth. That’s what our ancestors ate. That’s what our cells remember.
And if you’re eating processed ‘renal diets’ full of modified starches and artificial flavors… you’re not healing. You’re surviving on chemical ghosts.
Try this: one cup of bone broth daily. Skip the supplements. Let your body rebuild with what it recognizes. The numbers will follow.