When you're seriously ill, your body doesn't just feel tired-it changes how your hormones work. One of the most misunderstood patterns in medical labs is what happens to thyroid tests during severe illness. Many patients and even some doctors see low T3 or low T4 on a blood report and assume the thyroid is failing. But in most cases, the thyroid is perfectly fine. What’s really going on is sick euthyroid syndrome, a normal, adaptive response to stress-not a disease that needs treatment.
What Sick Euthyroid Syndrome Really Is
Sick euthyroid syndrome, also called nonthyroidal illness syndrome (NTIS), isn’t a problem with the thyroid gland at all. It’s your body slowing down its metabolism to survive. When you’re fighting sepsis, recovering from major surgery, or dealing with a severe burn, your body shifts energy away from non-essential functions. One of those functions is thyroid hormone conversion. This isn’t new. Doctors first noticed strange thyroid patterns in critically ill patients back in the 1970s. Since then, studies have shown that 70-75% of ICU patients have these abnormal thyroid test results. The higher the severity of illness, the more likely you are to see them. In sepsis, it’s present in 80-85% of cases. In diabetic ketoacidosis or major trauma, it’s over 60%. These aren’t lab errors. They’re biological signals.What the Lab Results Actually Show
The classic pattern of sick euthyroid syndrome is simple, but easy to misread:- Low T3-seen in 95% of cases. This is the most consistent sign.
- Low T4-in about half of severe cases.
- High reverse T3 (rT3)-up to 90% of patients. This is the inactive form of T3 that builds up when the body stops converting T4 properly.
- Normal or slightly off TSH-this is the key. In 60-70% of cases, TSH stays between 0.4 and 4.0 mIU/L. Sometimes it dips slightly below 0.4, or creeps up to 5-10 mIU/L during recovery. But it doesn’t go sky-high like in primary hypothyroidism.
Here’s why this matters: if your TSH is normal while T3 and T4 are low, you almost certainly have sick euthyroid syndrome-not an underactive thyroid. A low TSH with low T3/T4 would point to central hypothyroidism, which is rare and needs treatment. But in sick euthyroid syndrome, your pituitary gland isn’t failing-it’s just waiting for your body to recover.
Why Your Body Does This
Your body isn’t broken. It’s adapting. During serious illness, inflammatory chemicals like tumor necrosis factor-alpha, interleukin-1, and interleukin-6 surge. These cytokines directly interfere with how thyroid hormones are made, converted, and used. Type 1 deiodinase-the enzyme that turns T4 into active T3-slows down by 30-50%. At the same time, the enzyme that clears reverse T3 becomes less active, so rT3 piles up. Thyroid-binding proteins also drop slightly, meaning less hormone is bound and circulating. The result? Less active T3 reaches your cells. That’s intentional. Lower T3 reduces your metabolic rate by 15-20%. That saves energy. It helps your heart, lungs, and brain focus on survival instead of digestion, hair growth, or temperature regulation. As Dr. Yifan Xiao from Osmosis explains, this isn’t a malfunction-it’s a survival mechanism. In a study of ICU patients, those with the lowest T3 levels had higher mortality rates. But that’s because their illness was worse-not because low T3 killed them. The low T3 is a marker of severity, not the cause.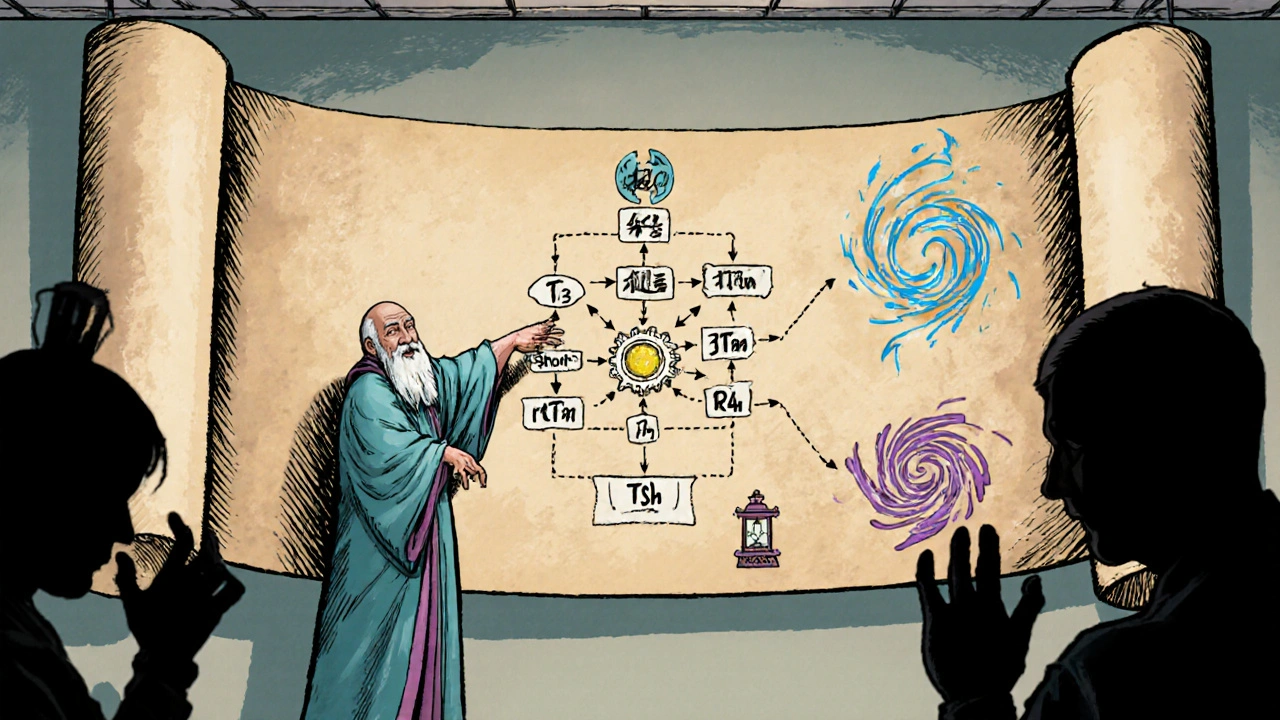
Conditions That Trigger It
Sick euthyroid syndrome doesn’t just happen in the ICU. It shows up in many serious conditions:- Sepsis-80-85% of patients
- Major surgery-65-70%
- Severe burns-75-80%
- Heart attack-50-55%
- Diabetic ketoacidosis-60-65%
- Anorexia nervosa-up to 90% in advanced cases
- Cirrhosis-70-75%
- Chronic kidney disease-60-65%
The pattern appears within 24 to 48 hours of the illness starting. It’s fast. It’s predictable. And it reverses as you recover. That’s why doctors don’t treat it.
It Looks Like Hypothyroidism-But It’s Not
Patients with sick euthyroid syndrome often feel like they have hypothyroidism: tired, cold, constipated, weak. But here’s the difference:- No weight gain or puffy face (no myxedema)
- No dry skin or hair loss
- No elevated thyroid antibodies (like TPO or TgAb)
- No enlarged thyroid gland
In true hypothyroidism, TSH is high, and antibodies are usually present. In sick euthyroid syndrome, TSH is normal or only slightly off, and antibodies are absent. If you’re sick and your doctor orders a thyroid panel, they should check for these clues before jumping to treatment.
Why Treating It Can Be Dangerous
Giving thyroid hormone to someone with sick euthyroid syndrome doesn’t help-it can hurt. A 2022 clinical trial with 450 critically ill patients compared those given levothyroxine with those given a placebo. The results? Identical 30-day mortality rates. Identical ICU stays. No benefit. No improvement. And that’s not an isolated finding. Multiple studies now show that giving thyroid hormones to these patients can increase the risk of heart rhythm problems, raise blood sugar, and even raise death risk by 8-10%. Why? Because you’re forcing a system that’s conserving energy to speed up-when it’s already under extreme stress. Dr. Anne R. Cappola from the University of Pennsylvania found that about 12% of ICU patients get unnecessary thyroid treatment because their labs are misread. That’s not just a waste of resources-it’s a real danger.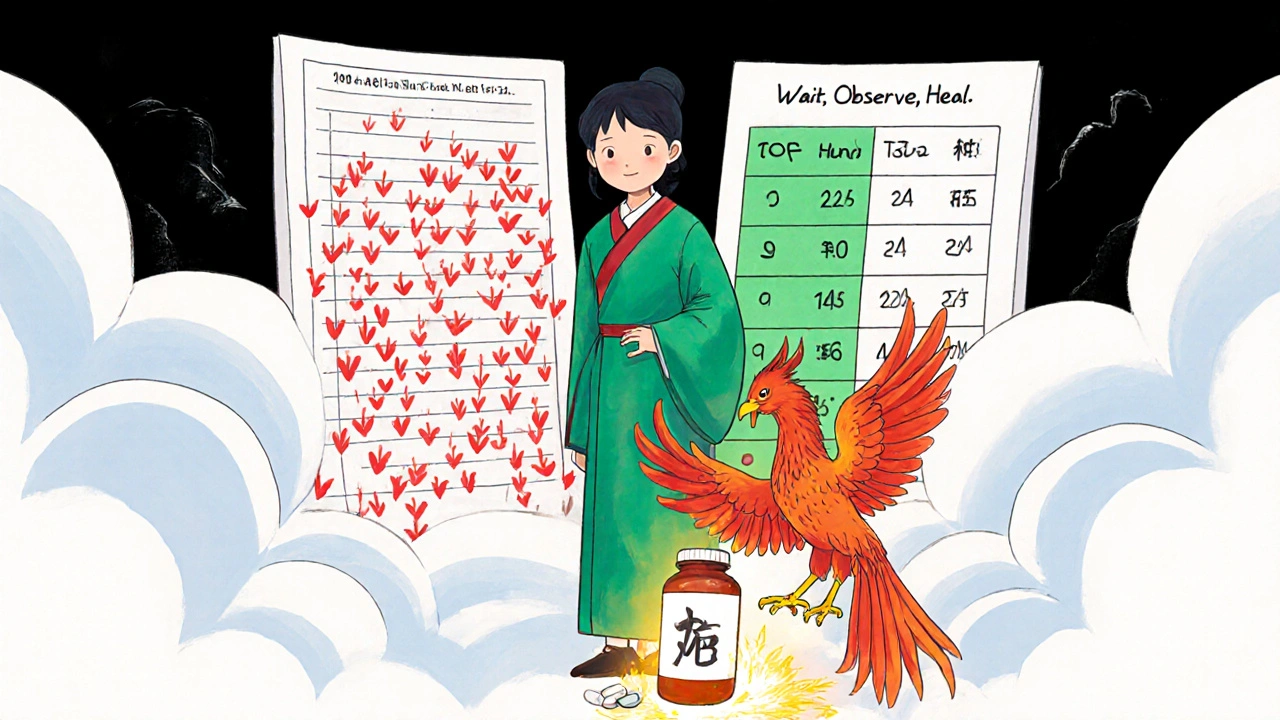
How Doctors Get It Right
The right diagnosis isn’t about one lab number. It’s about context:- Is the patient critically ill? If yes, abnormal thyroid tests are likely ESS.
- Is TSH normal or only mildly abnormal? Normal TSH with low T3 = ESS.
- Are thyroid antibodies present? If yes, it’s likely true autoimmune disease.
- Has the patient recovered from the illness? If not, wait.
The 2023 American Association of Clinical Endocrinology guidelines say: don’t test thyroid function in critically ill patients unless there’s a clear sign of thyroid disease-like a history of thyroid problems or a goiter. Most of the time, it’s just noise.
If thyroid tests were done during illness, repeat them 4-6 weeks after recovery. If hormone levels return to normal, ESS was the cause. If they stay low and TSH rises, then you’re dealing with true hypothyroidism.
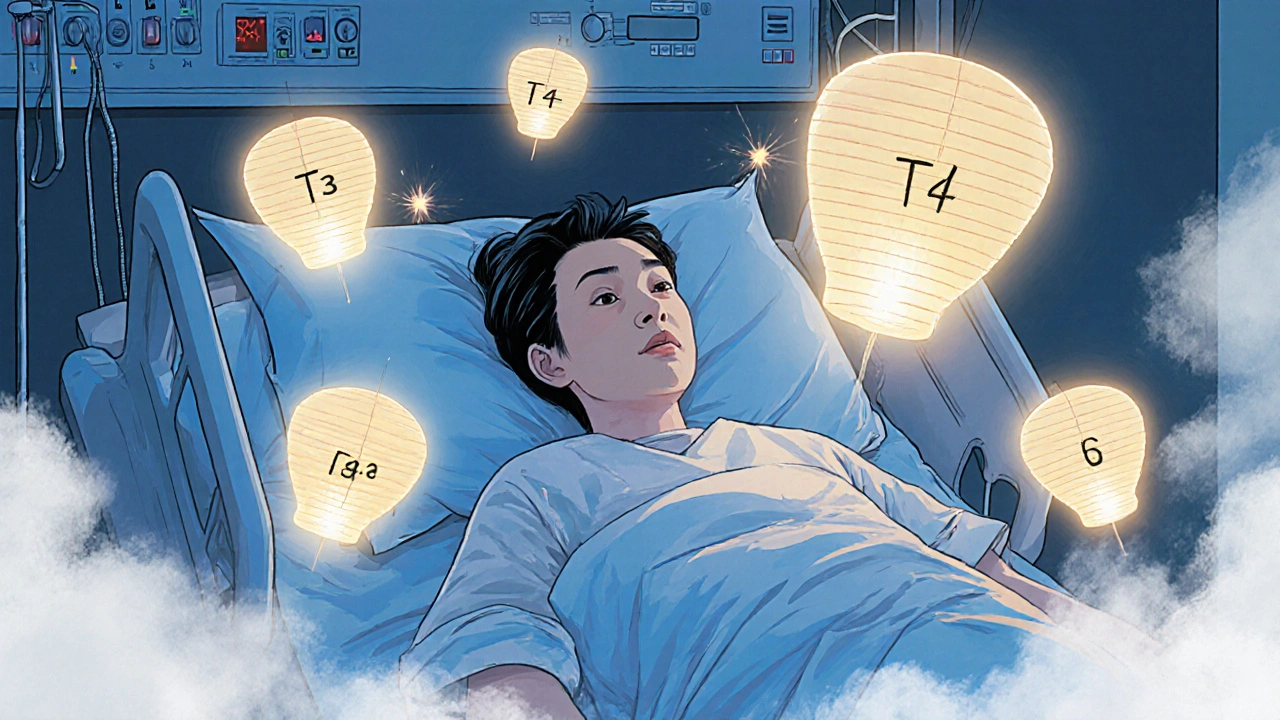
The Future: Using ESS as a Prognostic Tool
Doctors aren’t just ignoring ESS anymore-they’re learning to read it. A 2022 study in Critical Care found that patients with T3 levels below 40 ng/dL had a 45% chance of dying. Those with T3 above 80 ng/dL had only a 15% risk. That’s not a coincidence. T3 levels are becoming a tool to predict outcomes. The EUTHYROID-ICU study, led by Dr. Peter Laurberg in Denmark, is tracking over 2,500 ICU patients to see if specific patterns of thyroid hormone changes can predict who will recover quickly and who might need more support. Early data suggests that not just the level of T3, but how fast it drops and how long it stays low, may help guide care.What You Should Know
If you or someone you care about is hospitalized with a serious illness and thyroid tests come back abnormal:- Don’t panic. The thyroid is probably fine.
- Ask if the doctors have ruled out sick euthyroid syndrome.
- Don’t push for thyroid medication unless TSH is high and antibodies are present.
- Focus on treating the underlying illness-sepsis, heart failure, infection-not the lab numbers.
- Wait for recovery before retesting.
Sick euthyroid syndrome isn’t a diagnosis you need to fix. It’s a sign your body is fighting hard. And sometimes, the best medicine isn’t a pill-it’s time, rest, and letting your body heal on its own terms.
jim cerqua
November 21, 2025 AT 18:24This is the most important thing I've read all year. I had a friend in the ICU last year, doctors were ready to start her on levothyroxine because her T3 was 'abnormal'-like it was some kind of failure. She nearly got poisoned because no one knew this was normal. Sick euthyroid syndrome isn't a glitch-it's a survival mode. Your body isn't broken, it's just putting the car in neutral while the engine's on fire. And now I'm mad all over again.
They treat labs like gospel, but the human body isn't a spreadsheet. It's a warzone. And in war, you don't send more soldiers into the trench because the radio went silent-you fix the damn trench.
Also, why do we still let endocrinologists order thyroid panels on every feverish patient? It's like measuring the temperature of a burning building to decide if the fire alarm is working. The alarm is working. The building is on fire. Stop blaming the alarm.
I'm telling my doctor about this next time I go in. And if they still push meds? I'm walking out. No more lab-based witch hunts.
Someone needs to make a viral TikTok about this. Like, 'Your thyroid isn't broken, your life is.' With dramatic music and a guy in a lab coat crying in the corner.
God, I hate how medicine works sometimes.
Donald Frantz
November 23, 2025 AT 12:54Let’s be clear: this isn’t just a matter of misinterpretation-it’s systemic medical negligence. The fact that 12% of ICU patients are being given thyroid hormone unnecessarily isn’t a footnote, it’s a scandal. And the 2022 trial showing zero benefit with increased cardiac risk? That’s not just data-it’s preventable harm.
The AACE guidelines are right to say don’t test unless there’s a pre-existing condition. But why aren’t hospitals mandated to train staff on this? Why is this still considered 'advanced knowledge' instead of basic ICU protocol?
Every time a patient gets levothyroxine for sick euthyroid syndrome, they’re exposed to unnecessary risk. That’s not just poor judgment-it’s a failure of clinical education. We’re teaching residents to treat numbers, not patients. And that’s why people die.
Also, reverse T3 is the smoking gun. If your lab doesn’t measure it, they’re not doing the job. Demand it. Or demand a second opinion. This isn’t controversial-it’s evidence-based medicine 101.
Sammy Williams
November 23, 2025 AT 20:12Man, this is such a relief to read. I’ve been telling my mom for years that her 'hypothyroid' symptoms during chemo weren’t actually thyroid issues-just her body shutting down to fight cancer. She went through a whole year of unnecessary meds and side effects because no one explained this to her.
It’s wild how often we mistake adaptation for failure. Your body isn’t broken when it slows down-it’s being smart. Like when your phone goes into low-power mode. You don’t replace the battery, you just let it charge.
Thanks for putting this out there. I’m sharing this with my nurse friend. She’s gonna flip. We’ve all seen this happen too many times.
Also, the part about T3 levels predicting mortality? That’s next-level stuff. It’s not just about avoiding treatment-it’s about using the numbers as a warning sign. That’s the real win here.
Julia Strothers
November 24, 2025 AT 03:02Oh, so now the medical establishment is just going to ignore thyroid dysfunction because it’s 'convenient'? Classic. This is exactly how they cover up the truth. Why do you think they don’t want you to know about reverse T3? Because if people understood this, they’d realize the whole endocrine industry is built on misdiagnosing healthy people as 'hypothyroid' to sell pills.
And don’t get me started on Big Pharma’s role here. Levothyroxine is a billion-dollar product. You think they want doctors to stop prescribing it just because someone’s sick? No way. They’re funding studies that downplay this. The WHO is in on it too.
Look at the stats-70% of ICU patients? That’s not coincidence. That’s a pattern. And the fact that they’re pushing 'wait and see' instead of treating? That’s how they control the narrative. They want you dependent on meds, not empowered by knowledge.
They’ll say it’s 'normal adaptation'-but why is it only 'normal' when it benefits their profits? If your body adapts to starvation by slowing metabolism, they’ll call it anorexia. If it adapts to illness? Oh, it’s just 'sick euthyroid syndrome.' Convenient, isn’t it?
Wake up. This isn’t science. It’s corporate medicine.
Nikhil Purohit
November 24, 2025 AT 07:11This is gold. I’m an ICU nurse in Bangalore and we see this every week. Patients come in with sepsis, labs show low T3, family panics, doctors get pressured to prescribe Synthroid. I’ve had to explain this exact thing to families 20 times this year.
One guy’s daughter cried because she thought her dad was 'dying from thyroid failure.' I showed her the TSH was normal, the antibodies were zero, and explained how his body was conserving energy. She just hugged me. That’s the power of clear info.
Also, the reverse T3 point? So many labs here don’t even test it. We have to send samples to private labs in Mumbai. It’s a mess.
But honestly? I’m glad this is getting out. More docs need to know. Not just endocrinologists-ER nurses, med students, even paramedics. This isn’t niche knowledge. It’s life-saving.
Debanjan Banerjee
November 25, 2025 AT 18:51Let’s address the elephant in the room: sick euthyroid syndrome is not a 'syndrome' at all-it’s a physiological adaptation, and the term itself is misleading. The phrase 'euthyroid' implies the thyroid is functioning normally, which is technically true, but the entire construct is built on a misnomer. The correct term should be 'nonthyroidal illness-induced metabolic suppression' or something equally precise.
Furthermore, the literature consistently shows that the degree of T3 suppression correlates with cytokine load, not disease severity per se. TNF-alpha and IL-6 directly inhibit deiodinase type 1 expression via NF-kB pathways. This isn’t speculative-it’s molecular biology.
And while the 2022 trial showing no benefit from T4 replacement is compelling, it’s worth noting that the study population was heterogeneous. Future trials should stratify by baseline cytokine levels, duration of illness, and nutritional status. One-size-fits-all conclusions are dangerous.
Also, the use of reverse T3 as a prognostic marker is underutilized. A recent meta-analysis (2023, JCEM) showed that rT3/T3 ratio > 10 predicted 30-day mortality with 82% specificity. This should be incorporated into ICU scoring systems.
Finally, the AACE guidelines are a step forward, but they’re still reactive. We need proactive protocols: no thyroid testing in acute illness unless TSH > 10 or antibodies positive. Period. Education must begin in medical school, not residency.
Noah Fitzsimmons
November 25, 2025 AT 22:40Oh wow, so the thyroid is fine? That’s news to me. I guess I just wasted $1,200 on thyroid meds for the last 8 years because I thought I was 'hypothyroid' after my car accident. My bad. I should’ve known my body was just being 'adaptive' and not actually broken. Thanks for the enlightenment, Dr. Google.
Also, I’m pretty sure my cat has sick euthyroid syndrome. She’s been sleeping 20 hours a day since the vacuum cleaner came into the house. Clearly, she’s conserving energy. Maybe she needs a nap, not a pill. I’m calling her vet now.
Corra Hathaway
November 26, 2025 AT 18:42Yessssss! This is the kind of post that makes me believe in humanity again 😭👏
I’ve been screaming this from the rooftops since my mom had sepsis last year. Doctors were ready to put her on thyroid meds because her T3 was 'low.' I pulled up this exact article on my phone and read it to them. They paused. Then said, 'Huh. We didn’t know that.'
She didn’t get meds. She got rest. She got better. And now she’s back to gardening and yelling at the neighbor’s dog.
Also, the part about T3 levels predicting survival? That’s wild. I’m saving this to show my cousin who’s in the ICU right now. She’s terrified. This might give her hope.
Thank you for writing this. Seriously. The world needs more people who explain science like this-not like a textbook, but like a friend who’s been through it. 🫂