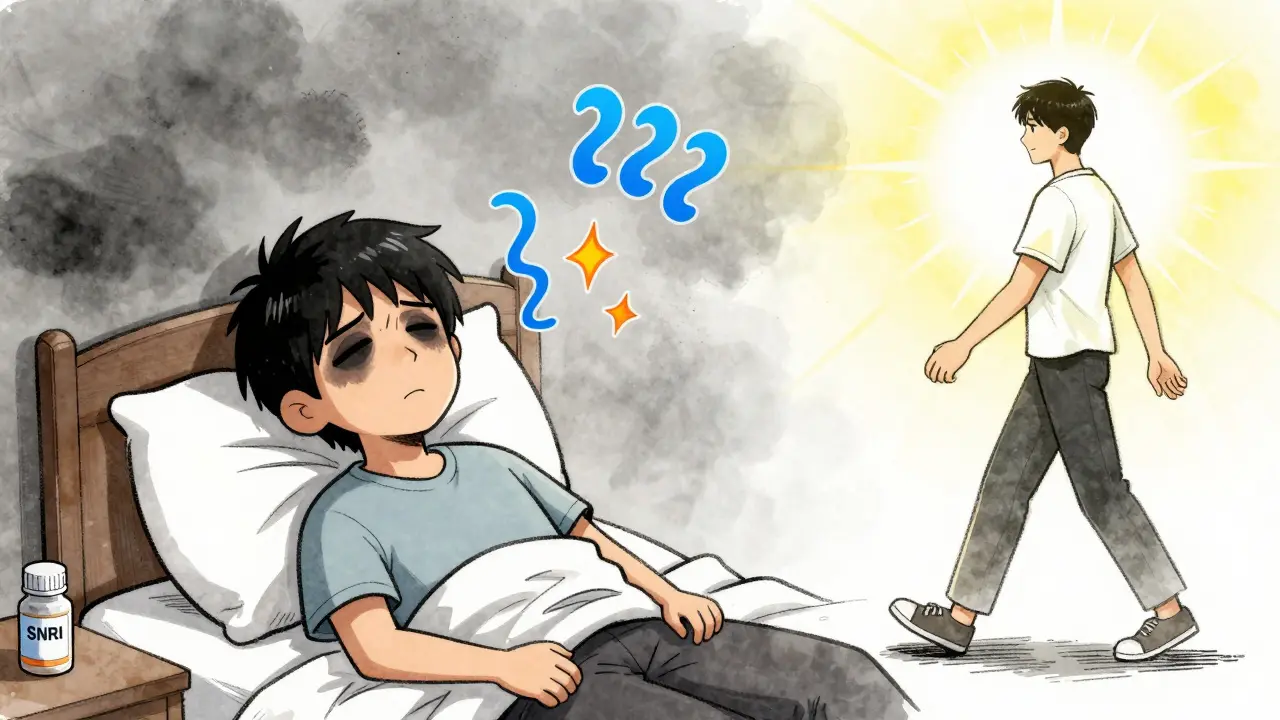
When antidepressants don’t work the first time, many people wonder what’s next. If SSRIs left you tired, numb, or still in pain, you’re not alone. SNRI medications offer a different path-one that doesn’t just lift mood but also tackles fatigue, brain fog, and chronic pain that often come with depression. These aren’t magic pills, but for a lot of people, they’re the missing piece.
How SNRIs Work Differently
SNRIs stand for Serotonin and Norepinephrine Reuptake Inhibitors. That’s a mouthful, but here’s what it really means: they boost two key brain chemicals-serotonin and norepinephrine-that help regulate mood, energy, focus, and even pain signals. Unlike SSRIs, which only touch serotonin, SNRIs hit both. That dual action makes a real difference for people who feel emotionally flat and physically drained.
Think of it like this: serotonin helps you feel calm and connected. Norepinephrine gives you drive and alertness. When both are low, you don’t just feel sad-you feel stuck. That’s why SNRIs often help people who’ve tried SSRIs and still can’t get out of bed, concentrate at work, or stop worrying about every little ache in their body.
The SNRIs You’re Likely to Encounter
In the U.S., four SNRIs are FDA-approved for depression:
- Venlafaxine (Effexor XR): The original SNRI, approved in 1993. Works differently at low vs. high doses-more like an SSRI at first, then adds norepinephrine as the dose increases.
- Duloxetine (Cymbalta, Drizalma Sprinkle): One of the most widely used. Approved not just for depression, but also for fibromyalgia, diabetic nerve pain, and chronic back pain.
- Desvenlafaxine (Pristiq): A metabolite of venlafaxine. Often prescribed for those who can’t tolerate the original.
- Levomilnacipran (Fetzima): The newest, with a stronger focus on norepinephrine. May help more with energy and motivation.
Duloxetine stands out because it’s the only one approved for physical pain conditions. If you’re dealing with arthritis, nerve pain from diabetes, or fibromyalgia, your doctor might choose it not just for your mood, but for your body too.
When Do They Start Working?
Don’t expect miracles in a week. Most people notice small improvements in sleep or energy after 2-3 weeks, but full effects usually take 4-6 weeks. For some, especially with chronic pain, it can take up to 12 weeks. That’s longer than people often expect.
That delay is frustrating, but it’s normal. The brain needs time to adjust. The key is sticking with it-if side effects aren’t unbearable, give it at least 6 weeks before deciding it’s not working.
Side Effects: What to Expect
SNRIs aren’t side effect-free. But they’re cleaner than older antidepressants like tricyclics, which caused dry mouth, constipation, and drowsiness in most users. With SNRIs, those problems are less common.
Here’s what you might actually experience:
- Nausea: Happens in about 25% of people on duloxetine. Usually fades after 1-2 weeks. Taking it with food helps.
- Dizziness or lightheadedness: Especially when standing up fast. Move slowly. Your body adjusts.
- Insomnia: More common with venlafaxine. Taking it in the morning helps.
- Sexual side effects: Lowered libido, delayed orgasm-reported in 20-30% of users. Not everyone gets this, but it’s real.
- Blood pressure rise: A small but real risk. About 5-8% of users see a noticeable increase. Doctors check BP at the start and again after 2-4 weeks.
One of the biggest concerns is withdrawal. If you stop suddenly, you might get “brain zaps”-electric shock-like sensations in your head-along with nausea, anxiety, or flu-like symptoms. That’s why tapering off slowly over 4-6 weeks is critical. Abrupt stops raise your risk of withdrawal by 28%. A gradual plan cuts it to under 10%.
How SNRIs Compare to Other Options
SSRIs like sertraline or escitalopram are still the first choice for most doctors. They’re gentler, with fewer side effects and lower risk of blood pressure spikes. But here’s the catch: about half of people on SSRIs don’t fully respond. That’s where SNRIs come in.
Studies show SNRIs have a slightly higher response rate-55-65% compared to 50-60% for SSRIs. But the real advantage isn’t just mood. For people with depression and chronic pain, SNRIs like duloxetine cut pain by 30-50% in 40-50% of users. Placebo only helped 20-30%. That’s not small.
And if you’re struggling with fatigue or lack of motivation? SNRIs often help more than SSRIs. One patient survey found 62% of people who switched from SSRIs to SNRIs felt more energy and better focus within 4-6 weeks.
Who Benefits Most?
SNRIs aren’t for everyone. But they’re a strong fit if you:
- Have tried one or two SSRIs and didn’t get better
- Feel physically exhausted, even when you sleep enough
- Have chronic pain-back pain, nerve pain, fibromyalgia, or arthritis
- Struggle with concentration or brain fog alongside low mood
- Have anxiety along with depression
Dr. David Mischoulon from Massachusetts General Hospital says SNRIs are especially helpful for people with “prominent fatigue or pain symptoms.” That’s not just a clinical observation-it’s what patients report over and over.
What About Cost and Access?
Venlafaxine and duloxetine are available as generics, which keeps costs down. In the U.S., a 30-day supply of generic venlafaxine XR can cost as little as $10-$20 with good insurance or discount cards. Duloxetine is a bit pricier but still under $30 for many.
Insurance often requires step therapy-meaning you have to try an SSRI first. But if you’ve already done that and it didn’t work, your doctor can appeal. Many insurers approve SNRIs after one failed SSRI.

Combining SNRIs With Other Treatments
Medication alone isn’t the whole story. A 2022 clinical trial found that 73% of people who took an SNRI and did cognitive behavioral therapy (CBT) went into full remission. That’s compared to just 48% on medication alone.
CBT helps you reframe negative thoughts. It gives you tools to cope when the medication hasn’t fully kicked in. It also helps prevent relapse after you stop taking the drug.
Even newer tools are helping. A 2023 study showed that people taking duloxetine while using a cognitive training app improved their memory and focus 35% more than those on the drug alone. Digital tools aren’t replacements-but they’re powerful supports.
What’s New in 2026?
The field is moving fast. In 2022, the FDA approved Drizalma Sprinkle-a powdered form of duloxetine-for children with anxiety disorders. That’s the first time an SNRI got pediatric approval beyond depression.
Genetic testing is becoming more common. Some labs now test for CYP2D6 and CYP2C19 gene variants, which tell your doctor how fast or slow your body breaks down SNRIs. If you’re a slow metabolizer, you might need a lower dose to avoid side effects. If you’re fast, you might need more. This testing isn’t perfect-but it’s helping 60-70% of patients find the right dose faster.
And research is looking at combining SNRIs with psychedelic-assisted therapy. Early trials show remission rates jump from 28% with SNRIs alone to 45% when paired with psilocybin therapy. These aren’t available yet, but they’re coming.
Final Thoughts
SNRIs aren’t the first step. But they’re one of the most useful second steps. If you’ve been stuck on an SSRI, feeling tired, in pain, or mentally foggy, it might be time to talk to your doctor about SNRIs. They’re not perfect. They have side effects. But for many, they’re the difference between surviving and finally feeling like yourself again.
The key is patience, communication with your provider, and not giving up too soon. If one SNRI doesn’t work, another might. And if you combine it with therapy or lifestyle changes? Your chances of real improvement go up significantly.
Are SNRIs better than SSRIs for depression?
Not always. SSRIs are usually tried first because they have fewer side effects. But if SSRIs don’t help enough-especially if you’re dealing with fatigue, pain, or poor concentration-SNRIs often work better. Studies show SNRIs have a slightly higher response rate (55-65% vs. 50-60%) and are more effective for depression with physical symptoms.
Can SNRIs help with chronic pain?
Yes. Duloxetine and venlafaxine are FDA-approved for diabetic nerve pain, fibromyalgia, and chronic musculoskeletal pain. Clinical trials show 30-50% pain reduction in 40-50% of patients, compared to 20-30% with placebo. For many, this pain relief is as important as the mood improvement.
How long does it take for SNRIs to work?
Most people notice small improvements in energy or sleep after 2-3 weeks. Full effects usually take 4-6 weeks, but for chronic pain or severe depression, it can take up to 12 weeks. Don’t stop too early-give it time.
What are the biggest risks with SNRIs?
The main risks are increased blood pressure (especially with venlafaxine), nausea early on, sexual side effects, and withdrawal symptoms if stopped abruptly. Blood pressure should be checked 2-4 weeks after starting. Never stop suddenly-taper slowly over 4-6 weeks to avoid brain zaps and other withdrawal effects.
Can I take SNRIs with therapy?
Absolutely. In fact, combining SNRIs with cognitive behavioral therapy (CBT) leads to remission in 73% of patients-compared to 48% with medication alone. Therapy helps you build skills that last beyond the medication. Many doctors now recommend this combo as standard care.
Prakash Sharma
January 8, 2026 AT 13:31SNRIs are just another Western scam pushed on developing nations. We don't need fancy pills to fix what's broken in our minds-our culture, our discipline, our yoga, our chai-those fix us. Why do we keep importing mental health trends like they're smartphones?
Manish Kumar
January 10, 2026 AT 03:20Think about it-serotonin and norepinephrine aren't just chemicals, they're metaphysical conduits of human will and emotional resonance. The brain isn't a circuit board, it's a symphony of ancestral memory and bioelectric longing. When SSRIs fail, it's not because the molecule didn't bind-it's because the soul wasn't ready to be lifted. SNRIs? They're the universe whispering back, 'You're not broken, you're just out of sync.' But only if you're willing to listen beyond the chemical noise.
Aubrey Mallory
January 10, 2026 AT 07:44For anyone struggling with chronic pain + depression, this is gold. I was on sertraline for 18 months and still couldn't get out of bed. Switched to duloxetine-within 5 weeks, my back pain dropped 40%, and I actually started cooking again. Not magic. Just science that finally matched my symptoms.
christy lianto
January 12, 2026 AT 01:17Just wanted to say-you’re not alone. I was on Effexor for 6 months. Nausea, insomnia, brain zaps when I tried to quit too fast. But when it finally clicked? I felt like myself for the first time in 5 years. It’s not easy. But it’s worth the grind. Keep going.
Dave Old-Wolf
January 13, 2026 AT 04:08So if SSRIs didn't work, SNRIs are next? What if neither work? Is there a third option? Just curious, not trying to be a jerk.
swati Thounaojam
January 14, 2026 AT 19:19my doc put me on pristiq and i cried for 3 days straight. then i slept 10 hours. then i got better. weird.
Luke Crump
January 16, 2026 AT 04:45Let me guess-this is the same ‘science’ that told us electroshock was the answer, then Prozac, then ketamine. Now SNRIs? What’s next-brain implants powered by TikTok? The pharmaceutical industry doesn’t cure people-it creates lifelong customers. Wake up.
Donny Airlangga
January 16, 2026 AT 09:47I had the brain zaps when I quit venlafaxine cold turkey. Worst week of my life. Now I taper over 8 weeks. No zaps. No panic. Just quiet. If you’re thinking of stopping-please, don’t wing it. Talk to your doc.
Molly Silvernale
January 18, 2026 AT 04:35SNRIs-serotonin, norepinephrine-two neurotransmitters dancing in the dark alleyways of the limbic system… and somehow, after 6 weeks of silent negotiation between synapses, the body whispers: ‘Ah. There you are.’ It’s not chemistry-it’s a conversation. And for once, the brain decided to answer.
Kristina Felixita
January 18, 2026 AT 18:05OMG this is so true!! I had fibro + depression and Cymbalta changed my life!! I can now walk to the mailbox without crying 😭 also, CBT + app training? YES!! I use Moodfit and my focus is like a laser now!! 💪🧠
Joanna Brancewicz
January 19, 2026 AT 14:36Pharmacokinetic variability via CYP2D6 polymorphisms significantly impacts SNRI efficacy and tolerability. Genotyping prior to initiation reduces adverse event burden by 40-60% in clinical cohorts.
Evan Smith
January 21, 2026 AT 07:19So… SNRIs are basically SSRIs but with extra caffeine? 😏 I mean, if I’m gonna feel wired and nauseous, at least let me get stuff done.
Lois Li
January 22, 2026 AT 21:55I switched from Lexapro to Fetzima after 2 years of feeling like a ghost. The energy boost wasn’t instant-but after week 5, I started walking my dog again. Small things. But they mattered. Thank you for writing this. I needed to see it.