Many people carry a label: sulfa allergy. But what does that actually mean? If you’ve been told you’re allergic to sulfa, you might have avoided medications like hydrochlorothiazide for high blood pressure, furosemide for fluid retention, or celecoxib for arthritis - even if you never had a real reaction. The truth? Most of those restrictions are unnecessary. The confusion around sulfa allergies isn’t just misleading - it’s dangerous. It leads to worse infections, longer hospital stays, and higher costs. And it’s all based on a misunderstanding of chemistry, not science.
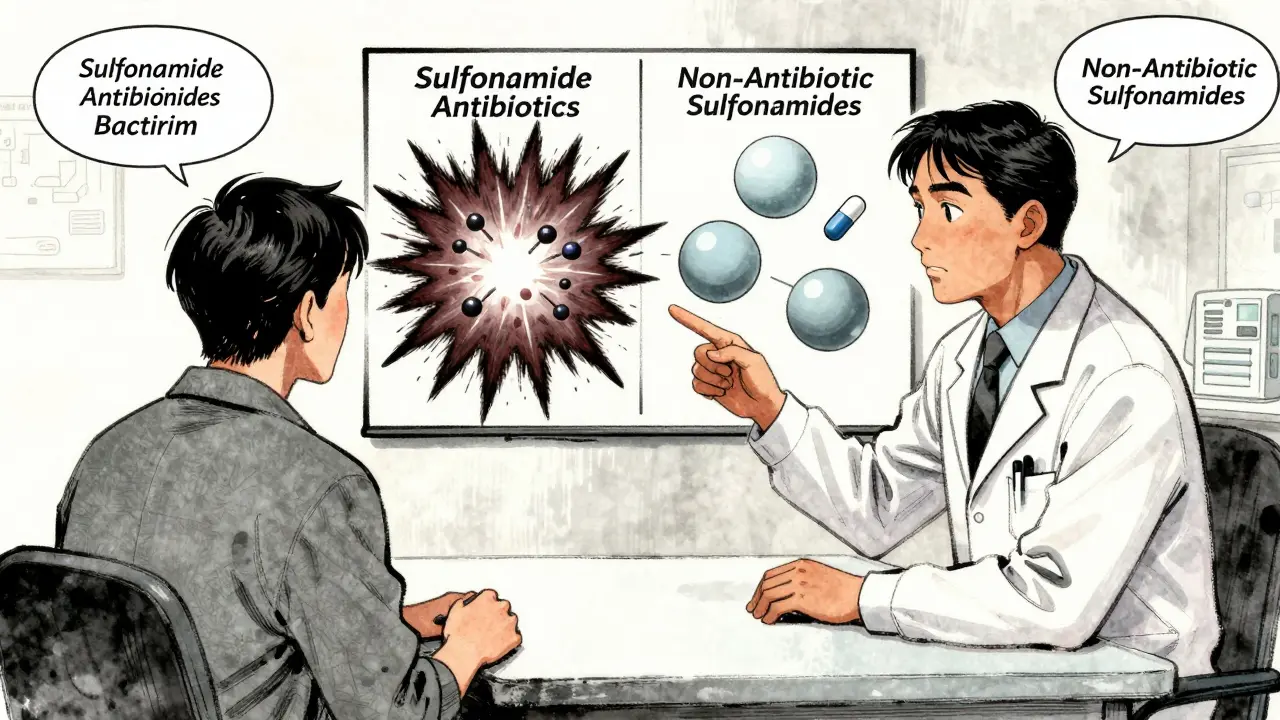
What Is a Sulfa Allergy, Really?
When someone says they have a "sulfa allergy," they usually mean they reacted to an antibiotic like sulfamethoxazole (found in Bactrim or Septra) or sulfadiazine. These are antimicrobial sulfonamides - drugs designed to kill bacteria. But "sulfa" doesn’t mean all drugs with sulfur. It’s not about the sulfur atom. It’s about a specific chemical structure: an aromatic amine group attached at the N4 position. This part breaks down in the body into a reactive compound called hydroxylamine, which can trigger an immune response in some people.That’s why only certain drugs are risky. If you had a rash, blistering, or worse after taking Bactrim, you likely have a true allergy - but only to similar antibiotics. You don’t need to avoid every drug with "sulf" in the name.
Which Medications Are Actually Risky?
If you have a confirmed allergy to an antimicrobial sulfonamide, you should avoid these:- Sulfamethoxazole (in Bactrim, Septra)
- Sulfadiazine
- Sulfacetamide (eye drops)
- Dapsone (used for leprosy and skin conditions)
- Sulfasalazine (Azulfidine) - this one’s tricky. It breaks down into sulfapyridine, which acts like an antibiotic. About 10% of people with sulfa antibiotic allergies react to it.
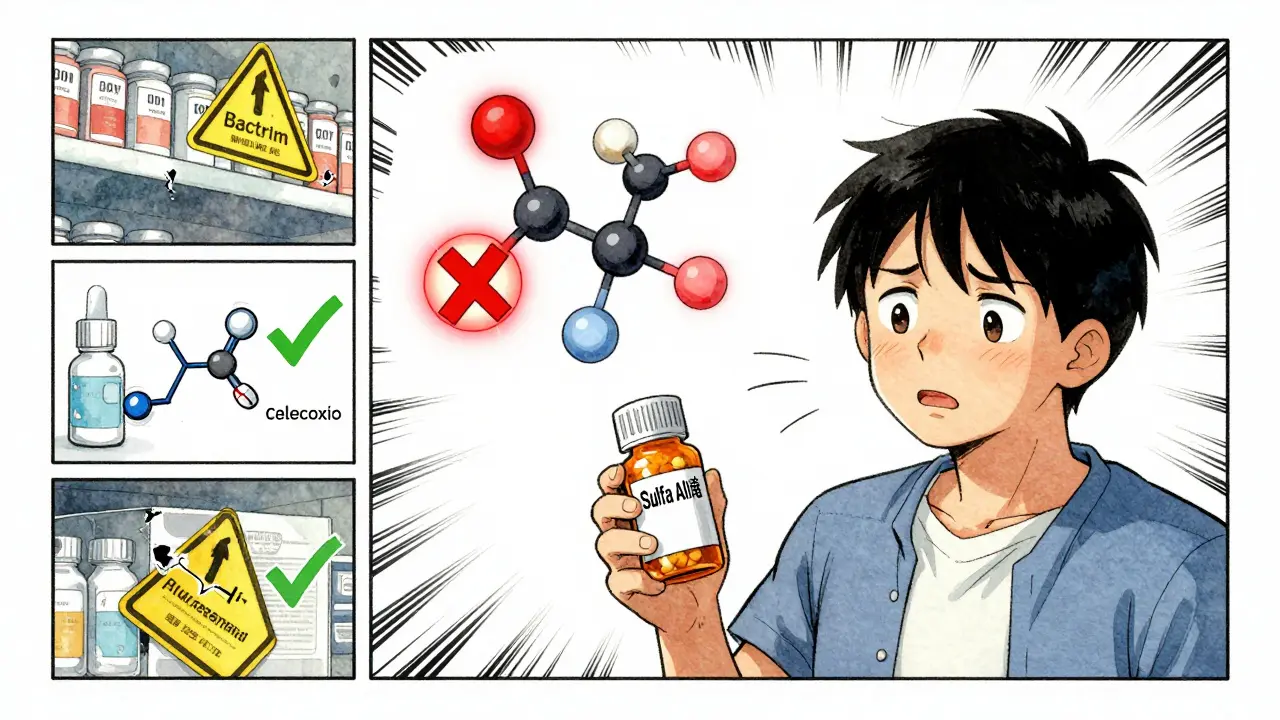
These are the drugs you can almost always take safely - even if you’ve had a serious reaction to Bactrim:
- Hydrochlorothiazide (HCTZ) - a common blood pressure pill
- Furosemide (Lasix) - used for heart failure and swelling
- Chlorthalidone - another diuretic
- Celecoxib (Celebrex) - for arthritis pain
- Sulfonylureas like glyburide - for type 2 diabetes
- Acetazolamide - for glaucoma and altitude sickness
Studies show that patients with true sulfonamide antibiotic allergies have no higher risk of reacting to these drugs than someone with no allergy at all. One study of 1,200 people with confirmed sulfa antibiotic allergies found only 0.8% had any reaction to non-antibiotic sulfonamides - the same rate as the general population.
Why the Confusion Exists
The problem started decades ago. When sulfonamide antibiotics were first used in the 1930s, they were the only sulfonamide drugs around. Doctors didn’t yet know about other types. So when patients had reactions, they were labeled "allergic to sulfa" - and the label stuck. Today, electronic health records still say "sulfa allergy" without distinguishing between antibiotic and non-antibiotic drugs. Pharmacists see it and assume the worst. Patients hear "avoid all sulfa drugs" and panic.Real-world data confirms the confusion. On patient forums, 63% of people who say they have a sulfa allergy avoid medications like hydrochlorothiazide or celecoxib - even though their doctors say it’s safe. One woman on Reddit took HCTZ for 15 years without issue, but her pharmacy still flagged it as "contraindicated." Another was denied furosemide for heart failure because of a rash she got from Bactrim 20 years ago.
And the consequences are serious. A 2022 report found that 12.3% of antibiotic errors in hospitals happen because doctors avoid sulfa drugs unnecessarily. Instead of prescribing a safe, targeted antibiotic like Bactrim for a UTI, they use something broader like ciprofloxacin. That increases the risk of deadly C. difficile infections by more than twice.
What About Other "Sulf" Things?
You might hear people say, "I’m allergic to sulfa, so I can’t eat sulfites in wine or take Epsom salts." That’s not true. Sulfites (used as preservatives), sulfates (like magnesium sulfate in Epsom salts), and even saccharin (Sweet’N Low) have nothing to do with sulfonamide antibiotics. They don’t contain the arylamine group. Your immune system doesn’t confuse them.If you reacted to wine or had a reaction to an IV magnesium sulfate, that’s not a sulfa allergy. It’s a different kind of reaction - maybe intolerance, maybe something else entirely. Don’t let misinformation stop you from using safe treatments.
How to Get It Right
If you’ve been told you have a sulfa allergy, here’s what to do:- Find out what you actually reacted to. Was it Bactrim? Sulfadiazine? Or something else? Write it down.
- Ask your doctor for clarification. Don’t let your record say "sulfa allergy." It should say "allergy to sulfonamide antibiotic" - and list the specific drug.
- Consider a drug challenge. If your reaction was mild (like a rash without fever or breathing trouble), your doctor can give you a single dose of hydrochlorothiazide or celecoxib under observation. Studies show 98.7% of people tolerate it without issue.
- Don’t assume you’re allergic to everything with "sulf" in the name. That includes diabetes pills, glaucoma drops, and heart medications.
For people who had severe reactions - like Stevens-Johnson Syndrome, toxic epidermal necrolysis, or DRESS syndrome - avoid all antimicrobial sulfonamides for life. But even then, non-antibiotic sulfonamides are still safe.
The Bigger Picture
This isn’t just about one drug class. It’s about how medicine handles labels. When we use vague terms like "sulfa allergy," we limit care. We increase costs. We make people sicker. The American College of Physicians, the Mayo Clinic, the Cleveland Clinic, and the American Academy of Allergy, Asthma & Immunology all agree: stop using "sulfa allergy" as a blanket term.Since 2022, major EHR systems like Epic have started splitting the label into two categories: "sulfonamide antibiotic allergy" and "non-antibiotic sulfonamide allergy." Hospitals that made this change saw a 42% drop in unnecessary allergy flags within six months. Pharmacists who took time to clarify allergies reduced inappropriate restrictions by nearly 70% - saving $287 per patient on average.
The financial impact? The U.S. spends $1.2 billion a year because of this confusion. That’s billions in extra hospital days, wrong antibiotics, and avoidable complications. Fixing this isn’t just smart medicine - it’s cost-saving medicine.
What’s Changing Now?
The FDA now requires drug labels to clearly distinguish between antimicrobial and non-antibiotic sulfonamides. In 2024, the Joint Commission made accurate allergy documentation a national patient safety goal. New diagnostic tools are emerging too - blood tests that detect IgE antibodies to the hydroxylamine metabolite can identify true sulfa antibiotic allergies with 94.7% accuracy.Still, a 2023 survey found that 67% of primary care doctors still believe non-antibiotic sulfonamides are risky for people with sulfa allergies. That’s why education matters. Clinicians need to understand the chemistry. Patients need to know their rights. And pharmacists need the tools to ask the right questions.
The message is clear: if you’ve been told you have a sulfa allergy, don’t accept it without details. Ask what drug caused the reaction. Ask if it was an antibiotic. Ask if you’ve ever tried a diuretic or arthritis pill safely. You might be avoiding medications you don’t need to avoid - and that could be making your health worse.
Can I take hydrochlorothiazide if I’m allergic to sulfa?
Yes, you can. Hydrochlorothiazide is a non-antibiotic sulfonamide. It lacks the specific chemical structure (arylamine group) that triggers allergic reactions in sulfonamide antibiotics. Studies show no increased risk of reaction in people with confirmed sulfa antibiotic allergies. Over 98% of patients who were challenged with hydrochlorothiazide after a prior sulfa antibiotic reaction tolerated it without issue.
Is celecoxib (Celebrex) safe for people with sulfa allergies?
Yes, celecoxib is safe. It’s a non-antibiotic sulfonamide used for pain and inflammation. Multiple studies, including one from the Mayo Clinic and another by the American College of Rheumatology, found no increased risk of allergic reactions in patients with sulfonamide antibiotic allergies. The odds of reacting to celecoxib are the same as someone with no allergy at all.
What’s the difference between sulfonamide antibiotics and other sulfonamides?
Sulfonamide antibiotics have a specific chemical group called an arylamine at the N4 position. This breaks down into hydroxylamine, which can trigger immune responses. Non-antibiotic sulfonamides like furosemide, hydrochlorothiazide, and celecoxib don’t have this group. They’re chemically different, so they don’t cause cross-reactions. The allergy is not to sulfur - it’s to a specific molecular shape found only in certain antibiotics.
Can I take Epsom salts or wine if I have a sulfa allergy?
Yes. Epsom salts contain magnesium sulfate, wine contains sulfites, and Sweet’N Low contains saccharin - none of these are sulfonamides. They don’t share the arylamine structure that causes sulfa antibiotic allergies. Reactions to these are unrelated and usually due to different mechanisms, like intolerance or sensitivity, not true allergy.
Should I get tested for a sulfa allergy?
If you have a vague history of a reaction - especially if it was mild - testing or a supervised drug challenge can be very helpful. Component-resolved diagnostics can now identify true sulfonamide antibiotic allergies with over 94% accuracy by detecting IgE antibodies to the hydroxylamine metabolite. Even without testing, a single-dose challenge with a non-antibiotic sulfonamide like hydrochlorothiazide is safe and can confirm tolerance.
What should I tell my doctor if I think I have a sulfa allergy?
Don’t just say "I’m allergic to sulfa." Say: "I had a reaction to [specific drug, e.g., Bactrim] when I was [age or year]. The reaction was [rash, hives, breathing trouble, etc.]." If you’re unsure, ask your doctor to check your medical records and consider a drug challenge. Accurate labeling helps you get better care and avoids unnecessary restrictions.
Diana Stoyanova
January 10, 2026 AT 01:44Okay but like… why are we still doing this? I had a rash from Bactrim in 2012 and spent 8 years avoiding HCTZ because my pharmacy flagged it. My BP was a nightmare. Finally asked my doctor to challenge me - took one pill, nothing happened. Now I’m on it daily. Why do we let outdated labels dictate our health? It’s not science, it’s superstition with a prescription pad.
tali murah
January 11, 2026 AT 12:21How is this even still a thing in 2024? The medical establishment has been correcting this since the early 2000s. Yet here we are - patients dying from C. diff because doctors are too lazy to read the damn chemistry. The fact that EHRs still lump ‘sulfa allergy’ as one monolithic red flag is criminal negligence. Someone should sue the vendors for malpractice-by-algorithm.
Jenci Spradlin
January 12, 2026 AT 05:40lol i got the bactrim rash too back in college. thought i was allergic to all sulfa stuff. turned out i was fine with celebrex and lasix. my pharmacist still argues with me though. like bro its not even the same molecule. how hard is it to google ‘sulfonamide chemistry’?
Elisha Muwanga
January 12, 2026 AT 15:28It’s no surprise. American medicine is built on fear, not facts. We’ve turned every minor reaction into a life-altering label. Meanwhile, countries like the UK and Germany have clear guidelines and far fewer medication errors. We don’t need more drugs - we need better education. And maybe less reliance on overworked pharmacists who don’t have time to read the fine print.
Maggie Noe
January 13, 2026 AT 02:44OMG YES. 😭 I took hydrochlorothiazide for 10 years before someone told me I had a ‘sulfa allergy’ - and I never had a problem. My doctor just shrugged and said ‘it’s fine.’ Why do we let fear override science? This is why people distrust medicine - because we’re given nonsense labels instead of real info. 🙏
Gregory Clayton
January 14, 2026 AT 07:52Bro. My grandma got denied lasix for her heart failure because she had a rash from sulfa antibiotics 30 years ago. She ended up in the ER. The nurse said ‘we don’t give sulfa drugs to people with sulfa allergies.’ I had to pull up the Mayo Clinic study on my phone and read it to her. That’s not healthcare. That’s bureaucratic horror.
Catherine Scutt
January 15, 2026 AT 08:55People who say they’re ‘allergic to sulfa’ without knowing which drug caused it? You’re not brave. You’re just lazy. If you don’t know your own medical history, don’t blame the system. Go dig up your records. Talk to your doctor. Stop being a walking medical myth.
Darren McGuff
January 16, 2026 AT 19:26As a pharmacist in the UK, I see this daily. We have a ‘sulfa antibiotic’ flag in our system - everything else is clearly labeled. It’s not hard. The technology exists. The training exists. What’s missing is the will. I’ve had to explain this to doctors who still think furosemide is risky. It’s exhausting. But someone has to do it.
Ashley Kronenwetter
January 18, 2026 AT 19:09Thank you for this clear, evidence-based breakdown. The distinction between antimicrobial and non-antibiotic sulfonamides is not only chemically accurate but clinically essential. I encourage all clinicians to update their documentation and educate their patients. Precision in language saves lives.
Aron Veldhuizen
January 20, 2026 AT 11:48Let’s be honest - this isn’t about chemistry. It’s about control. The pharmaceutical industry profits from broad-spectrum antibiotics. If everyone could safely use Bactrim for UTIs instead of cipro, their margins shrink. The ‘sulfa allergy’ myth keeps people on expensive, overprescribed drugs. It’s not ignorance. It’s incentive.
Heather Wilson
January 20, 2026 AT 15:04Interesting. But let’s not pretend this is new. The literature has been clear since the 1990s. The fact that 67% of primary care doctors still misunderstand this speaks to a systemic failure in continuing medical education. And yet, we keep blaming patients for being misinformed. The real failure is institutional. The data? Solid. The implementation? Broken.
Micheal Murdoch
January 20, 2026 AT 16:27If you’ve been told you have a ‘sulfa allergy’ - don’t panic. Don’t assume. Ask. What drug? What happened? When? Was it a rash? A fever? Trouble breathing? Write it down. Then ask your doctor: ‘Can we test this?’ or ‘Can I try a non-antibiotic sulfa drug under supervision?’ Most of you will be fine. And if you are? You just got your health back. That’s not magic. That’s medicine.