Treatment-Resistant Depression: What Works When Antidepressants Fail
When someone has treatment-resistant depression, a form of major depressive disorder that doesn’t improve after trying at least two different antidepressants at adequate doses and durations. Also known as refractory depression, it affects about 30% of people with depression and isn’t a sign of weakness—it’s a biological reality that needs different tools. Most people start with SSRIs like sertraline or fluoxetine, but if those don’t lift the fog after 6–8 weeks, the problem isn’t motivation. It’s chemistry. The brain’s serotonin, norepinephrine, or dopamine systems may not be responding the way they should, or other factors like inflammation, thyroid issues, or even sleep disorders are quietly keeping the depression stuck.
That’s where antidepressants, medications designed to alter brain chemicals to improve mood. Also known as antidepressive agents, they include not just SSRIs but also SNRIs, MAOIs, and atypical options like bupropion come into play differently. Switching isn’t always the answer. Sometimes adding another drug—like lithium or thyroid hormone—helps boost the effect. Other times, it’s time to step outside the pill bottle. ketamine, a fast-acting anesthetic now used off-label for severe depression. Also known as esketamine, it works through glutamate pathways instead of serotonin, offering relief in hours instead of weeks has changed the game for many. Then there’s electroconvulsive therapy, a procedure that triggers controlled seizures to reset brain activity. Also known as ECT, it’s one of the most effective treatments for severe, unresponsive depression, even if it still carries stigma. These aren’t last resorts—they’re valid, evidence-backed options that should be discussed early, not only after years of trial and error.
What you’ll find in the posts below isn’t just a list of drugs. It’s real-world insight into how medications like SSRIs can mess with sleep, why some side effects are predictable and others aren’t, and how things like circadian rhythm or liver function can change how your body handles treatment. You’ll see how generic versions affect long-term costs, how drug interactions can make things worse, and why some people respond to one thing and not another. This isn’t theory. It’s what people actually experience when standard care doesn’t cut it—and what comes next when it doesn’t.
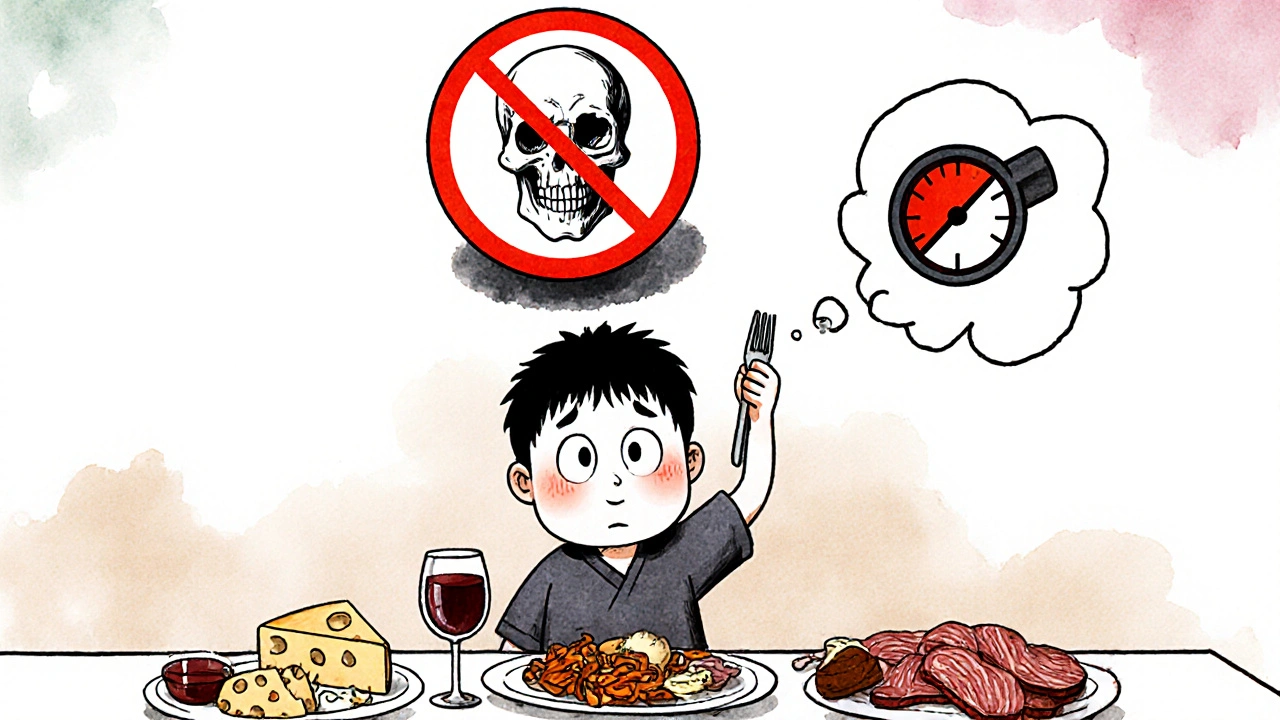
Monoamine Oxidase Inhibitors: What You Must Know About Side Effects and Dietary Restrictions
MAOIs are powerful antidepressants for treatment-resistant depression, but they come with strict dietary rules and dangerous drug interactions. Learn the real risks, how to stay safe, and why they still matter.