When your doctor orders a TSH and T4 test, it’s not just another blood draw. It’s a window into how your entire metabolism is functioning. For millions of people, especially women over 40, these two numbers can explain why they’re exhausted, gaining weight, or feeling cold when everyone else is fine. Yet, too many patients are left confused because their TSH is "normal" but they still feel awful. That’s because understanding thyroid function isn’t about one number-it’s about how TSH and T4 work together, and when to look beyond them.
What TSH and T4 Actually Measure
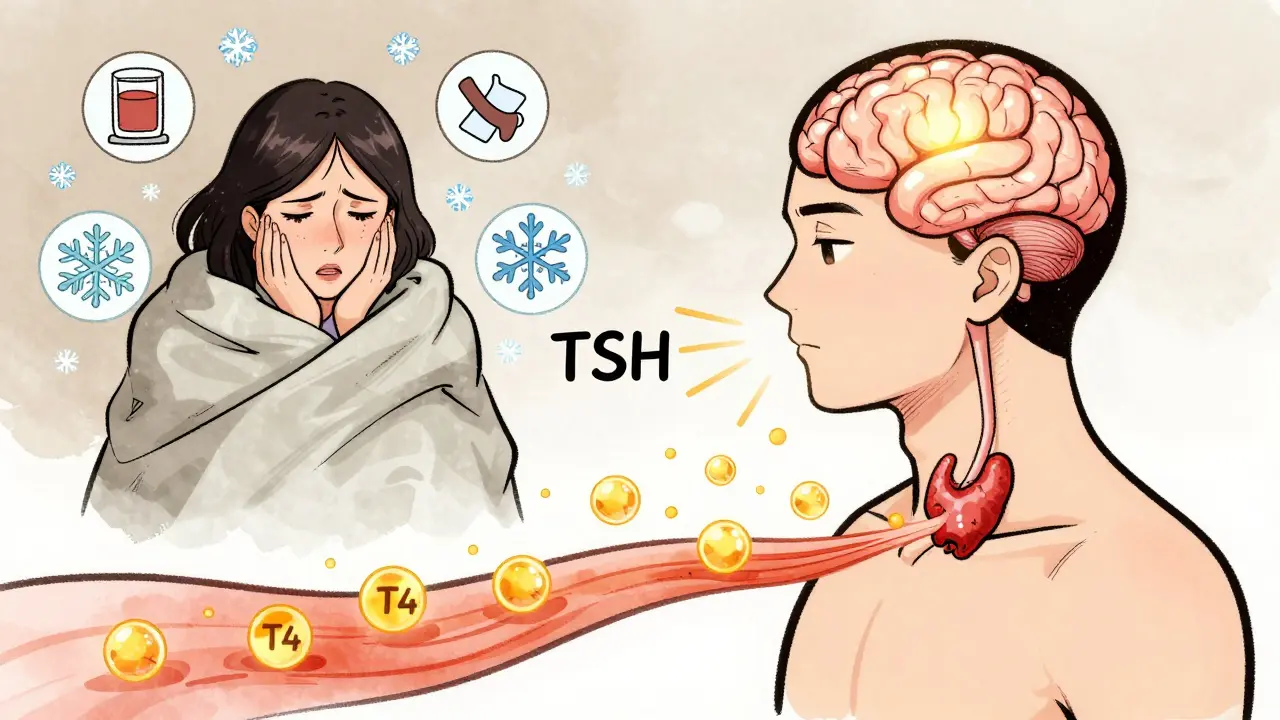
Thyroid-stimulating hormone (TSH) is made by your pituitary gland, the control center in your brain. Its job? To tell your thyroid: "Make more thyroid hormone." T4, or thyroxine, is the main hormone your thyroid produces. Most of it gets converted into T3, the active form that powers your cells. But T4 is what gets measured because it’s stable, abundant, and easier to test.
The classic rule is simple: if your thyroid isn’t making enough T4, your pituitary pumps out more TSH to try to fix it. That’s why high TSH usually means underactive thyroid (hypothyroidism). If your thyroid is overproducing, TSH drops like a stone. That’s hyperthyroidism.
But here’s the catch: TSH alone misses about 5-7% of thyroid problems. A 2020 meta-analysis of over 128,000 patients showed that using TSH alone catches 75% of thyroid disorders. Add free T4, and that jumps to 98%. That’s why guidelines from the American Thyroid Association say: TSH first, then free T4 if TSH is off.
Normal Ranges Aren’t One-Size-Fits-All
You might see a lab report saying your TSH is 4.2 mIU/L and think, "That’s within normal limits." But normal isn’t always optimal. The traditional range of 0.5 to 5.0 mIU/L was set decades ago and includes people with undiagnosed thyroid issues. Modern endocrinology suggests tighter targets.
For most healthy adults, the ideal TSH range is 0.5 to 2.5 mIU/L-especially if you’re on levothyroxine. A 2023 survey of over 12,500 patients on ThyroidChange.org found that those with TSH between 0.5 and 2.5 reported significantly better energy, mood, and weight control than those with TSH at 3.5 or higher-even if it was "normal."
Age changes everything. In people over 70, a TSH up to 6.5 mIU/L can be normal. The American Association of Clinical Endocrinologists updated their guidelines in 2021 to reflect this. Older adults often have slower metabolism and don’t need the same thyroid hormone levels as a 30-year-old. Pushing TSH too low in seniors can raise heart risks.
Pregnancy is another world entirely. In the first trimester, TSH should be under 2.5 mIU/L. Why? Because your baby’s brain depends on your thyroid hormone until 12 weeks. The Endocrine Society’s 2023 guidelines say: if you’re pregnant and your TSH is above 2.5, you need treatment-even if your free T4 is normal.
Free T4 vs. Total T4: Why It Matters
Not all T4 tests are created equal. Total T4 measures all the hormone in your blood-including the part stuck to proteins. But only the "free" part (free T4 or FT4) can enter your cells and work. That’s why doctors almost always order free T4, not total T4.
Here’s why: estrogen, pregnancy, liver disease, and even birth control pills change the protein levels that bind T4. So your total T4 might look high, but your free T4 is actually low. That’s a classic trap. A 2021 study in Thyroid journal found that 15-20% of patients had misleading total T4 results because of these binding proteins.
Free T4 normal range is typically 0.7 to 1.9 ng/dL. But here’s another twist: different labs use different machines. Roche’s test might read 1.5 ng/dL, while Siemens’ test on the same blood sample reads 1.3 ng/dL. That 12% variation, reported in Clinical Chemistry in 2021, can lead to unnecessary dose changes if your lab switches.
Diagnosing Hypothyroidism and Hyperthyroidism
Let’s break down the real diagnostic patterns:
- Primary hypothyroidism: TSH >4.5 mIU/L + FT4 <0.8 ng/dL. This is Hashimoto’s, the most common cause. You need levothyroxine.
- Subclinical hypothyroidism: TSH 4.5-10 mIU/L + normal FT4. Some doctors treat this, especially if you have symptoms or high thyroid antibodies. Others wait. The decision depends on age, heart health, and how you feel.
- Hyperthyroidism: TSH <0.1 mIU/L + FT4 >1.8 ng/dL. This is Graves’ disease or a toxic nodule. Needs antithyroid drugs, radioiodine, or surgery.
- Central hypothyroidism: TSH <0.5 mIU/L + low FT4. Rare. Caused by pituitary or hypothalamus damage. Often missed because TSH looks "low" instead of high.
And here’s a hidden problem: non-thyroidal illness. If you’re in the ICU, recovering from surgery, or fighting a bad infection, your TSH can drop and your FT4 can look low-even if your thyroid is fine. This is called "euthyroid sick syndrome." In these cases, treating with thyroid hormone can hurt you. That’s why ICU doctors check FT4 even if TSH is normal.
How Levothyroxine Dosing Works
Levothyroxine is the standard treatment for hypothyroidism. The starting dose? About 1.6 mcg per kilogram of body weight. So a 70 kg (154 lb) person starts around 112 mcg per day. But that’s just a guess.
Older adults, people with heart disease, or those who’ve had a heart attack? Start lower-0.5 to 0.7 mcg/kg. Too much too fast can trigger arrhythmias.
Children? They need way more per kilogram. Infants start at 10-15 mcg/kg/day. That’s because their brains are growing fast. Missing this window can cause permanent developmental delays.
After starting levothyroxine, you wait six weeks before checking TSH again. Why? It takes that long for your body to fully adjust. If TSH is still high, you increase the dose by 12.5-25 mcg. If it’s too low, you cut it back. Once stable, you test once a year.
But here’s what patients don’t tell doctors: symptoms don’t always match TSH. A 2023 trial in The Lancet Diabetes & Endocrinology found that 15-20% of people on levothyroxine still had fatigue, brain fog, or weight gain-even with perfect TSH and FT4. That’s why some endocrinologists now check FT3 in these cases. It’s not routine, but it’s becoming more common.
Why Patients Get Lost in the System
Thyroid patients are some of the most frustrated in medicine. A 2023 survey of 12,500 people found that 68% waited over a year to get diagnosed because their TSH was "normal" but they were clearly unwell. One woman in Edinburgh told her GP she couldn’t get out of bed for months. Her TSH was 4.1. Her doctor said, "It’s fine. You’re just stressed." She waited 22 months before a new doctor checked her free T4-it was 0.6 ng/dL. She started levothyroxine and felt like herself again in six weeks.
Another issue? Lab variation. If your TSH jumps from 2.8 to 4.2 after switching labs, your doctor might think you need more medicine. But it’s not your thyroid-it’s the machine. The FDA’s new harmonized reference material (NIST SRM 2921), approved in 2024, is meant to fix this. It’s already cutting lab-to-lab variation from 15% to under 5%.
And then there’s the AI revolution. Mayo Clinic’s 2024 pilot program used machine learning to analyze TSH, FT4, age, BMI, and symptoms. It reduced misdiagnoses by 22%. That’s huge. In the next five years, this kind of tool could become standard-helping doctors see what the numbers alone can’t.
What You Should Ask Your Doctor
If you’re being tested for thyroid issues, here’s what to say:
- "Can we check free T4, not just TSH?"
- "What lab do you use? Can I get the same one for follow-ups?"
- "Is my TSH in the optimal range for my age and health?"
- "If I’m on levothyroxine, what’s my target TSH?"
- "Could my symptoms be thyroid-related even if my numbers are "normal"?"
Don’t accept "it’s normal" if you don’t feel normal. Thyroid disease is common, treatable, and often misunderstood. You deserve better than a one-number diagnosis.
What’s Next for Thyroid Testing
The TSH/FT4 combo isn’t going away. It’s still the gold standard. But the future is personalization. The American Thyroid Association’s 2025 guidelines (in draft) will likely recommend FT3 testing for patients with persistent symptoms despite normal TSH and FT4. Antibody tests (like TPOAb) are already used to confirm Hashimoto’s-but they don’t guide treatment. Reverse T3? Still not proven useful in routine care.
Point-of-care TSH tests exist-they give results in 15 minutes. But they cost $2,500 for the machine and $15 per test. Most clinics stick with central labs because they’re cheaper and more accurate.
For now, the best advice is simple: TSH is your first clue. Free T4 is your second. Together, they tell the real story. Don’t let a single number define your health. If you’re still tired, cold, or gaining weight despite "normal" labs, push for more. Your thyroid is trying to tell you something.
Meenal Khurana
February 3, 2026 AT 23:58My TSH was 4.8 last year. Doctor said 'it's fine.' I felt like a zombie. Started taking levothyroxine. Three weeks later, I slept through my alarm for the first time in years-and it wasn't because I was tired.
Just saying.
Joy Johnston
February 5, 2026 AT 01:23Thank you for this exceptionally clear breakdown. As a clinical endocrinologist, I can confirm that the 0.5–2.5 mIU/L target for euthyroid patients on levothyroxine is increasingly supported by evidence, particularly in symptomatic individuals. The outdated 5.0 upper limit persists largely due to inertia in primary care protocols.
Additionally, the lab variability issue is critically underdiscussed. A shift from Roche to Siemens assays can falsely suggest 'under-treatment'-leading to unnecessary dose escalation and iatrogenic hyperthyroidism. Always request your lab’s reference range and assay type.
For pregnant patients: TSH >2.5 is not borderline-it’s clinically significant. Fetal neurodevelopment is non-negotiable.
Shelby Price
February 5, 2026 AT 18:33So… if my TSH is 3.1 and I’m tired all the time, does that mean I’m just… not normal? 😅
Also, why do labs never tell you which machine they used? Seems like a big deal.
Keith Harris
February 6, 2026 AT 21:06Oh please. This is the same tired, overhyped thyroid dogma peddled by wellness influencers and naturopaths who think your thyroid is a magic switch. TSH is the gold standard. If your labs are normal, you’re not hypothyroid-you’re just lazy, stressed, or eating too many carbs.
And don’t get me started on 'optimal ranges.' That’s not medicine, that’s astrology with a lab coat. I’ve seen patients go from 0.5 to 0.1 TSH because some blog told them to-and then they ended up with atrial fibrillation. Thanks for nothing, Dr. Oz.
Mandy Vodak-Marotta
February 8, 2026 AT 07:43Okay, so I’ve been on levothyroxine for 7 years and my TSH hovers between 2.3 and 2.8. I feel great. My energy? Perfect. My weight? Stable. My mood? Actually happy.
But my doctor keeps trying to bump my dose down because ‘it’s still above 2.5’-like I’m some kind of metabolic criminal. I’ve had three different endos over the years and they all say the same thing: ‘If you feel good, don’t fix it.’
Meanwhile, my cousin’s TSH is 1.2 and she’s jittery, losing hair, and can’t sleep. So yeah, numbers mean nothing without context. Also, why does everyone act like free T4 is some secret code? It’s literally just the part that works. Like, duh.
And the lab variability thing? I had my blood drawn at two different hospitals in the same week. Same day, same time, same phlebotomist. One said 1.4, the other said 1.8. I called the lab. They said, ‘Yeah, we switched vendors last month.’ No warning. No explanation. Just… here’s your new normal. Thanks, healthcare system.
Also, why do we still use ng/dL? Why not pmol/L? Why do we still use mIU/L? Why not μIU/mL? Why is everything in this field so archaic? I just want to know what’s going on in my body without feeling like I’m decoding hieroglyphics.
rahulkumar maurya
February 10, 2026 AT 00:20How quaint. You all speak of 'optimal ranges' as if you’ve read the original papers from the 1990s NIH consensus panel. The 0.5–2.5 range? That’s not evidence-based-it’s a marketing ploy by pharmaceutical companies pushing T4 monotherapy. Real endocrinologists know that T3/T4 combination therapy is superior for 30–40% of patients, yet you’re all still clinging to TSH like it’s scripture.
And don’t even get me started on 'free T4'-a misnomer if ever there was one. The assay measures only a fraction of bioavailable hormone. Reverse T3? Thyroid antibodies? TSH receptor stimulators? You’re all missing the forest for the trees.
My TSH is 4.1. I feel amazing. My T3 is high-normal. My reverse T3 is low. My antibodies? Negative. So yes, I am hypothyroid. But not by your outdated criteria. By mine. And mine are based on actual physiology, not lab reports.
Alec Stewart Stewart
February 10, 2026 AT 01:26Hey, just wanted to say this is super helpful. I’ve been feeling off for years and finally got tested last month. My TSH was 3.9, T4 was 0.9. My doctor said 'wait and watch.' I felt like giving up.
Reading this made me realize I’m not crazy. I’m not lazy. My body’s just not getting the signal it needs.
Thanks for explaining the lab stuff so clearly. I’m going to ask for a free T4 next time-and also ask what machine they use. 😊
Geri Rogers
February 10, 2026 AT 22:28OMG YES. I’ve been screaming this for years. My TSH was 4.7 and my doctor laughed. Said I was 'too young' to be hypothyroid. I was 32. I had no energy, my hair was falling out in clumps, and I was cold in a 75-degree room.
I went to a functional medicine doc. They did a full panel: TSH, free T4, free T3, reverse T3, TPO, TGAb. Turns out my TPO was through the roof. I had Hashimoto’s. Started on levothyroxine. Within 6 weeks, I cried because I could lift my arms without feeling like I was dragging anvils.
And the lab thing? I switched from Quest to LabCorp and my 'normal' T4 went from 1.5 to 1.1. I nearly had a panic attack. My dose didn’t change. My body didn’t change. Just the machine. 🤯
Also, if you’re pregnant and your TSH is over 2.5? GET TREATED. Your baby’s brain is literally building itself right now. Don’t wait for symptoms. Don’t wait for 'normal.' Be the mom who says NO.
Janice Williams
February 11, 2026 AT 23:21This is precisely the kind of pseudoscientific, emotionally manipulative drivel that has turned thyroid health into a cult. TSH is the most sensitive, specific, and validated marker in all of endocrinology. To suggest that 'optimal' ranges are anything other than marketing is dangerous. You’re encouraging patients to self-medicate, ignore evidence, and chase phantom symptoms.
And the idea that lab variability is a crisis? That’s like saying your scale is unreliable because it reads 150.2 one day and 150.7 the next. It’s noise. It’s not pathology.
People who feel 'off' with normal labs have anxiety, depression, or poor sleep hygiene. Not thyroid disease. Stop blaming your hormones for your life choices.
Justin Fauth
February 13, 2026 AT 08:58Let’s be real: if you’re American and you’re tired, you’re not hypothyroid-you’re just soft. Back in my day, we didn’t have labs. We had grit. We woke up at 5 a.m., worked 12 hours, and didn’t whine about our TSH.
Now everyone wants a pill for their feelings. You’re not 'exhausted'-you’re lazy. You’re not 'cold'-you’re out of shape. You’re not 'gaining weight'-you’re eating junk and scrolling TikTok all day.
And don’t get me started on 'free T4.' That’s just fancy jargon for 'I want a prescription.'
Stop medicalizing normal human fatigue. We’re not broken. We’re just weak.
Amit Jain
February 15, 2026 AT 04:27My mom had thyroid issues in India. Doctor tested only TSH. She felt bad for 3 years. Then we went private. Free T4 was low. Started medicine. She’s fine now.
Don’t trust only TSH. Always ask for free T4. Simple.
Harriot Rockey
February 16, 2026 AT 15:37This is the most helpful thing I’ve read all year. I’ve been on levothyroxine for 5 years and my doctor always says 'you’re fine' when my TSH is 2.7. But I’m not fine. I’m tired. My skin is dry. I cry for no reason.
I just asked for a full panel. My T3 was low. My reverse T3 was high. My doctor said, 'We don’t test that.' I’m going to a new one tomorrow. 🙌
Also, the lab variability thing? I had blood drawn at the same hospital twice in two months. Same phlebotomist. Different results. I printed both and showed them. They apologized. Said they switched machines. No one told me. I felt like a lab rat.
Thank you for validating what I’ve been feeling. I’m not crazy. I’m just not being heard.
Demetria Morris
February 18, 2026 AT 00:34It’s irresponsible to suggest that 'normal' lab ranges are arbitrary. The guidelines exist for a reason. If you’re not meeting clinical criteria for hypothyroidism, you do not have hypothyroidism. Period.
Encouraging patients to chase 'optimal' levels based on anecdotal blogs is not medicine-it’s self-indulgent delusion. You’re not helping. You’re harming.
And for the love of science, stop using emoticons in medical discussions. It undermines credibility.
Prajwal Manjunath Shanthappa
February 19, 2026 AT 09:25...I see you’re all still clinging to the outdated, Western-centric dogma of TSH-centric diagnostics... as if the human endocrine system were a machine calibrated solely by American lab standards... while ignoring the vast literature on thyroid hormone transporters, deiodinase polymorphisms, and cellular resistance mechanisms that have been established since 2018...
...and yet, you still believe that a single serum concentration of T4-measured by an instrument with a 12% inter-assay variability-can define your metabolic fate...?
...how quaint.
...perhaps you should consult the 2022 meta-analysis in Nature Reviews Endocrinology on tissue-specific thyroid hormone action... before prescribing levothyroxine like it’s a vitamin...
...or are you too busy scrolling through Reddit to read peer-reviewed literature?...
Joy Johnston
February 20, 2026 AT 13:21Just to clarify: I didn’t say TSH is the only thing that matters. I said it’s the best initial screen. But when symptoms persist despite 'normal' TSH, you don’t stop there-you dig deeper. That’s not 'chasing phantoms.' That’s being a good doctor.
And yes, free T4 matters. And yes, lab variability matters. And yes, pregnant women need tighter targets.
And no, I’m not a 'wellness influencer.' I’m a board-certified endocrinologist who’s seen too many patients suffer because their doctors didn’t look beyond the reference range.
So if you’re going to call this 'pseudoscience,' at least cite a guideline that contradicts the American Thyroid Association’s 2023 update. Or better yet-share your data.