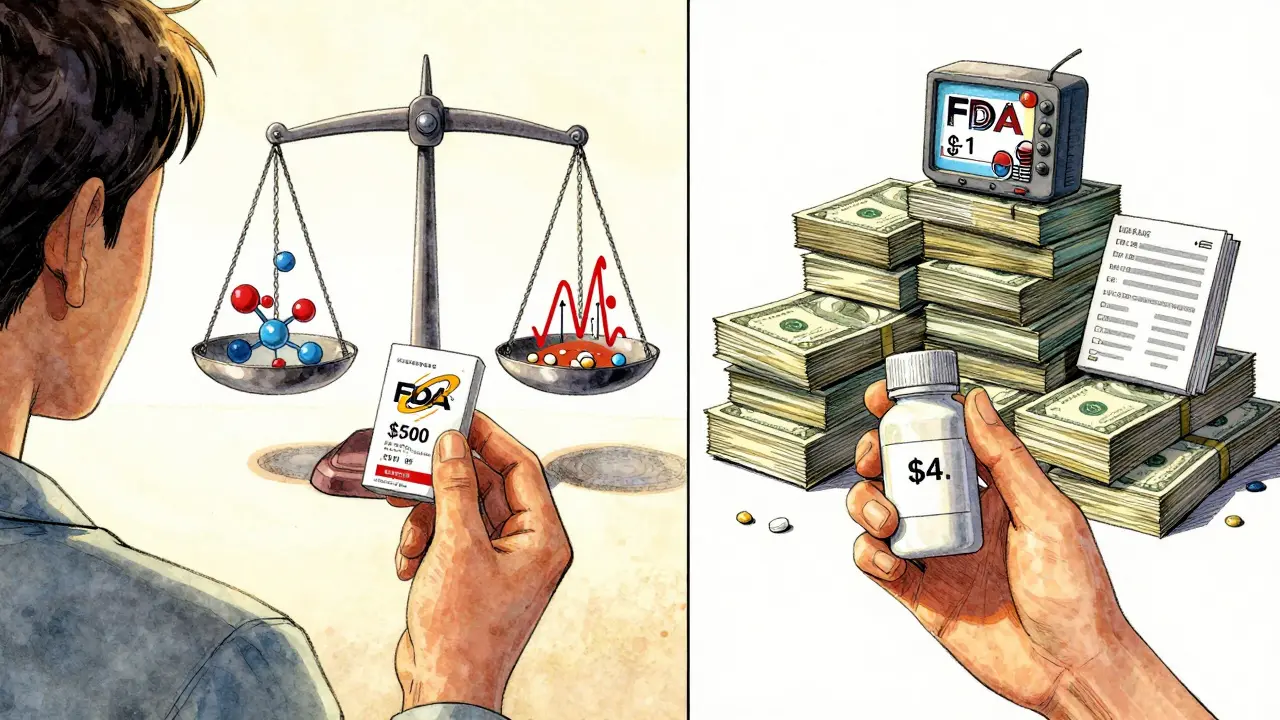
Ever looked at your pharmacy receipt and wondered why a generic pill costs $4 while the brand-name version costs $500? It’s not a scam. It’s not a trick. It’s the system working exactly as designed - and it’s saving Americans billions every year.
Same Medicine, Different Price Tag
A generic drug isn’t a weaker version. It’s not a copycat. It’s not a knockoff. It’s the exact same active ingredient, in the same strength, delivered the same way. If your doctor prescribes atorvastatin for cholesterol, the generic version does the same job as Lipitor. Omeprazole works the same as Prilosec. Levothyroxine replaces Synthroid without changing your thyroid levels. The U.S. Food and Drug Administration (FDA) requires generics to prove they deliver the same amount of medicine into your bloodstream at the same rate as the brand-name drug. That’s called bioequivalence. The acceptable range? Between 80% and 125% of the brand’s blood concentration. That’s tight. That’s science. That’s not luck. So why the huge price difference?The $2.6 Billion Hurdle
Brand-name drug companies spend an average of $2.6 billion to bring a new drug to market. That’s not a typo. That’s what the Tufts Center for the Study of Drug Development found in 2014. Where does that money go? - 8 to 12 years of research and testing- Hundreds of clinical trials involving thousands of patients
- Failed experiments - most drugs never make it past early stages
- Marketing, legal teams, patent filings, and lobbying All of that is paid for by the monopoly period. Once a drug gets FDA approval, the company gets 20 years of patent protection from the date they first filed. That’s their chance to recoup everything - and then some. During those 20 years, no one else can sell the same drug. No generics. No competition. No price drops.
How Generics Skip the Cost
Generic manufacturers don’t have to repeat any of that. They don’t need to run new animal studies. They don’t need to fund Phase 1, 2, or 3 clinical trials. The FDA already knows the drug works. The safety profile is known. The dosage is proven. Instead, they file what’s called an Abbreviated New Drug Application (ANDA). It’s a shorter, cheaper, faster path. The entire process takes 1 to 3 years - not 10 to 15. The cost? Around $1 million to $5 million per drug. That’s less than 0.2% of what the brand-name company spent. And here’s the kicker: the FDA still inspects their factories. Just like brand-name makers, generic manufacturers must follow the same strict rules - Current Good Manufacturing Practices (CGMP). The FDA does about 12,000 inspections a year worldwide. If a generic plant fails, it’s shut down. Same as Pfizer or Merck.
Competition Drives Prices Down
Once a patent expires, the floodgates open. The first generic maker gets a 180-day head start. Then others come in. Soon, you’ve got 10, 14, even 20 companies selling the same pill. That’s when prices really drop. The Congressional Budget Office found that within the first year of generic entry, prices fall by 80% to 90%. By year three, they’re often 95% lower than the brand. Take atorvastatin. When Lipitor’s patent expired in 2011, dozens of companies started making it. Today, a 30-day supply costs $4 at Walmart. The brand? Still priced at $500 - and almost no one buys it anymore.Why You Still See Brand-Name Drugs
You might still see ads for brand-name drugs. You might still hear your neighbor say, “I only take the real thing.” That’s not because generics are less effective. It’s because of marketing. Brand companies spend billions on TV ads, doctor visits, and patient programs. They want you to believe their pill is better. But the data says otherwise. A 2023 Tebra survey of 1,000 Americans found that 84% of people believe generics are just as effective. Yet 62% still trust the brand more. Why? Because they’ve seen the ads. Because they remember the logo. Because they don’t know the science. Even worse - some patients report side effects after switching. But that’s rarely because the medicine changed. It’s because the pill looks different. A generic might be blue instead of orange. Smaller. Bigger. Different shape. That freaks people out. They think, “This isn’t the same.” The FDA’s “Know Your Meds” campaign was launched in 2023 to fix this. Pharmacists are now trained to explain: “The medicine inside is identical. Only the color, shape, or filler changed.”Who Saves the Most?
The real winners? Patients. Insurance companies. Medicare. Medicaid. In 2022, generic drugs made up 90.5% of all prescriptions filled in the U.S. But they only accounted for 18% of total drug spending. Brand-name drugs? Just 9.5% of prescriptions - but 82% of the cost. That means for every $100 spent on prescriptions, $82 goes to brands. $18 goes to generics. And that $82 is mostly wasted on marketing, patent extensions, and profit margins - not better medicine. From 2007 to 2016, generics saved the U.S. healthcare system $1.67 trillion. In 2022 alone, they saved $293 billion. That’s enough to cover free healthcare for millions.
What About Complex Drugs?
Some drugs are harder to copy. Inhalers. Creams. Injectables. Biologics. These aren’t simple pills. They’re complex formulas. That’s why biosimilars - the generic version of biologic drugs - are still rare. But the FDA is working on it. In 2023, they released new guidance to speed up approval of complex generics. Their goal? Cut approval time from 5 years to 2. That could save another $50 billion a year. And yes - for drugs with a narrow therapeutic index, like warfarin or levothyroxine, some doctors prefer to stick with one brand. Why? Because tiny changes in blood levels can matter. But even here, the FDA says: if the generic is approved, it’s safe. Switching between different generic manufacturers is still considered safe - as long as the FDA approved them all.What You Can Do
You don’t need to be a pharmacist to save money. Here’s how:- Ask your doctor: “Is there a generic version?”
- Check your insurance formulary. Generics are almost always Tier 1 - $0 to $15 copay.
- If your pharmacy switches your drug without telling you, ask why. You have the right to request the brand - but you’ll pay more.
- Use apps like GoodRx or SingleCare. They show you the lowest cash price, even for brand-name drugs.
- Don’t assume a higher price means better quality. The pill inside is identical.
The Bigger Picture
The generic drug industry isn’t just about saving money. It’s about access. Without generics, millions of people couldn’t afford their medications. Diabetics. Heart patients. People with depression. Asthma. High blood pressure. A 2023 report from RxOutreach showed that patients who switched to generics saved an average of $317 per month. That’s rent. That’s groceries. That’s not choosing between medicine and food. And it’s not going away. By 2028, over 150 brand-name drugs will lose patent protection - with combined sales of $157 billion. That means more generics. Lower prices. More people treated. The system works. It’s not perfect. But it’s the reason you can buy 30 days of metformin for $4 instead of $400. It’s the reason your grandfather takes his blood pressure pill every day. It’s the reason you’re not bankrupt because of a prescription. Generics aren’t cheaper because they’re worse. They’re cheaper because we stopped paying for things that don’t matter - like advertising, patent extensions, and monopoly pricing. And that’s a win for everyone.Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove bioequivalence - meaning they deliver the same amount of medicine into your bloodstream at the same rate. Studies show no difference in effectiveness for the vast majority of medications. Over 90% of prescriptions filled in the U.S. are generics, and they work just as well.
Why do generic pills look different from brand-name pills?
U.S. trademark laws prevent generic manufacturers from making pills that look identical to brand-name drugs. That means color, shape, size, and inactive ingredients (like fillers or dyes) can differ. But the active ingredient - the part that treats your condition - is exactly the same. If you’re confused by a change in appearance, talk to your pharmacist. They can confirm it’s the same medicine.
Can switching to a generic drug cause side effects?
Side effects from switching are rare and usually not caused by the medicine itself. Most often, they’re due to psychological factors - like worrying the drug isn’t working - or changes in inactive ingredients that affect how the pill dissolves in your stomach. For most people, switching causes no issues. For drugs with a narrow therapeutic index (like warfarin or levothyroxine), doctors may recommend staying on one version. But switching between FDA-approved generics is still considered safe.
Why are generic drugs so much cheaper if they’re the same?
Brand-name drugs cost billions to develop because companies must pay for years of research, clinical trials, and marketing. Generic manufacturers skip all that. They don’t repeat expensive tests because the FDA already approved the original drug. Their costs are only $1-5 million per drug, not $2.6 billion. Plus, once multiple companies start making the same generic, competition drives prices down - often by 80-90%.
Is it safe to take generics made in other countries?
Yes. The FDA inspects all manufacturing facilities - whether they’re in the U.S., India, China, or elsewhere - to make sure they meet the same strict quality standards. About 70% of active pharmaceutical ingredients come from India and China, but every facility is subject to FDA inspections. If a factory fails, it’s shut down. The location doesn’t affect safety - only whether the facility passes FDA inspection.
Jodi Harding
January 18, 2026 AT 21:47Generics are the quiet heroes of modern medicine. I used to think brand-name was better until my dad switched to generic metformin and his blood sugar stabilized. Same pill. Same results. Just no $500 monthly bill.
Danny Gray
January 19, 2026 AT 20:05Let’s be real - the real scam isn’t the price difference. It’s that we let pharmaceutical companies turn medicine into a luxury product. They didn’t invent diabetes. They just figured out how to charge you for breathing.
Aysha Siera
January 19, 2026 AT 23:32Did you know most generics are made in China and India? The FDA says it’s safe but they also let companies lie about their inspections. You think your $4 pill is clean? Think again. Your body is a lab rat for global supply chains.
rachel bellet
January 20, 2026 AT 12:55While the bioequivalence thresholds are statistically valid, they ignore intra-individual variability and pharmacokinetic outliers. The 80–125% AUC range is a regulatory artifact, not a clinical guarantee. For drugs with narrow therapeutic indices, the assumption of interchangeability is methodologically flawed and potentially hazardous.
Pat Dean
January 22, 2026 AT 10:21Why do Americans think they deserve cheap medicine? Other countries don’t get this luxury. We’re the ones funding the R&D. If you want cheap pills, move to India. Then complain when your local clinic runs out of everything.
Jay Clarke
January 23, 2026 AT 23:50My grandma took Lipitor for 10 years. Switched to generic after her husband died. Said the pill tasted different. Started crying every time she took it. Not because it didn’t work - because it reminded her he was gone. Medicine isn’t just chemistry. It’s memory. And sometimes, the brand is the only thing left.
Selina Warren
January 24, 2026 AT 07:50Stop being passive. If you’re paying $500 for a pill, you’re being played. Go to Walmart. Buy the generic. Tell your doctor you’re done being a cash cow. This isn’t healthcare - it’s corporate extortion. Wake up. Fight back. Your life isn’t a profit margin.
Andrew Qu
January 25, 2026 AT 06:19For anyone worried about switching - I’m a pharmacist with 12 years in community care. I’ve seen thousands of patients switch from brand to generic. The vast majority have zero issues. The ones who complain? Usually the ones who saw the ad for the brand. The pill doesn’t change. The fear does. Talk to your pharmacist. Ask them to show you the FDA bioequivalence report. It’s not magic. It’s math. And it’s on your side.