Every year, more than 1.5 million people in the U.S. end up in the emergency room because of something as simple as taking the wrong pill. Not because they were careless - but because the system failed them. Medication errors aren’t rare mistakes. They’re systemic problems that kill, hospitalize, and drain billions from healthcare budgets. And yet, most people don’t realize how deeply this affects public health - until it happens to someone they know.
Medication Errors Are a Silent Epidemic
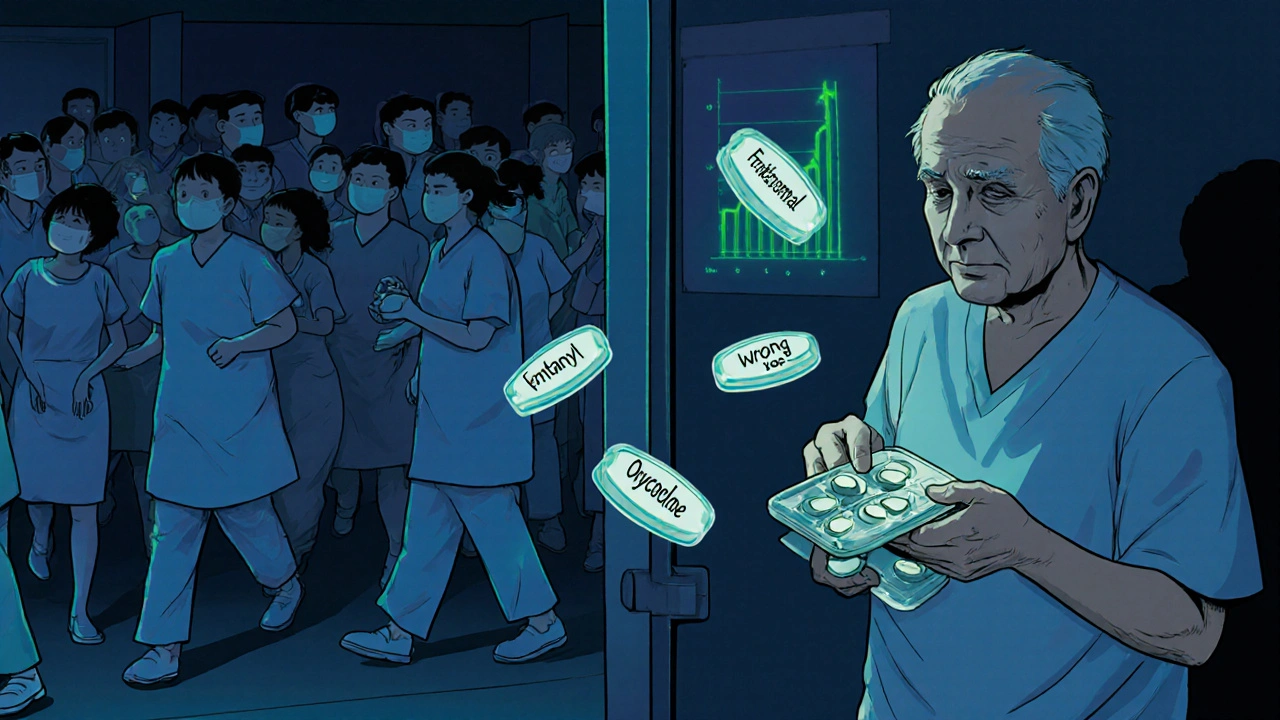
The World Health Organization says 1 in every 10 patients in high-income countries suffers harm from unsafe medication use. That’s not a statistic from a decades-old study - it’s from 2025 data. These aren’t just typos on prescriptions. They’re wrong doses, drug interactions, mislabeled pills, and confusion over discharge instructions. In the U.S. alone, medication errors cost $42 billion annually. That’s more than the entire healthcare budget of many small countries. The numbers get worse when you look at who’s most at risk. Older adults take an average of four prescriptions a day. By 2030, one in five Americans will be over 65. That means more drugs, more chances for something to go wrong. And it’s not just seniors. Fentanyl-laced counterfeit pills are now the leading cause of death for Americans between 18 and 45. In 2023, the DEA seized over 80 million of these fake tablets. Many people think they’re taking oxycodone - they’re not. They’re taking a lethal dose of fentanyl, often without knowing.Why This Isn’t Just a Hospital Problem
Most people assume medication safety is something hospitals handle. But the truth? Most errors happen outside the hospital. About 70% of preventable adverse drug events occur in outpatient settings - at pharmacies, in patients’ homes, during transitions from hospital to home. Think about this: You’re discharged after a heart attack. You get a list of six new medications. The doctor says, “Take one in the morning, one at night.” But the handwriting is messy. The pharmacist calls to clarify - but the nurse didn’t document the change in the system. You get home. You’re tired. You mix up the pills. Two days later, you’re back in the ER with dangerously low blood pressure. This isn’t hypothetical. A 2024 study of 15,000 patient transitions found that two out of three had at least one unintentional medication error. And it’s not just about confusion. The FDA’s MAUDE database recorded over 200 deaths and 1,900 injuries from infusion pump errors between January 2023 and August 2024. These are machines meant to deliver precise doses - but software glitches, poor design, and lack of training turned them into weapons. One nurse told Reddit: “I’ve seen a pump deliver 10 times the dose because the screen didn’t update after the nurse changed the setting.”Technology Can Help - But Only If It Works Right
There are tools that work. Barcode scanning at the bedside cuts administration errors by 86%. Electronic prescribing with clinical decision support reduces prescribing mistakes by 55%. AI systems can now predict which patients are at highest risk for adverse events with 73% accuracy. But here’s the problem: Most hospitals have these tools - but they don’t talk to each other. Your EHR doesn’t sync with the pharmacy system. The pharmacy system doesn’t update your primary care doctor. A 2024 study found that only 63% of U.S. hospitals had fully compliant health IT systems under the 21st Century Cures Act. That means even when technology exists, it’s often broken by design. And it’s not just hospitals. Independent doctors’ offices - where most prescriptions are written - are far behind. Only 42% of them have any kind of medication safety system in place, according to the Medical Group Management Association. Meanwhile, big hospital systems spend millions on AI and automation. The gap between big and small providers is widening.
Adherence Is the Real Bottleneck
You can have the perfect prescription - but if the patient doesn’t take it, it’s useless. The WHO says improving adherence may have a greater impact on population health than any single medical treatment. And yet, only about 75% of people with high blood pressure or diabetes take their meds as prescribed. Why? Cost. Complexity. Side effects. Confusion. A 2025 PharmD Live report found that patients who got a visual medication schedule - a simple chart with pictures of pills and times - were 38% more likely to take them correctly. Another study showed that patients who used a digital portal to track their meds had 29% better adherence. But here’s the kicker: Most patients don’t even know they’re supposed to ask questions. A 2024 American Hospital Association survey found that 76% of patients had communication problems about their medications during hospital stays. And 32% didn’t understand their discharge instructions. That’s not patient negligence - that’s system failure.What’s Working - And What’s Not
Some places are getting it right. The Netherlands reduced medication errors by 44% by mandating electronic prescribing across every pharmacy and clinic. The UK’s National Reporting and Learning System helped cut serious errors by 30% by making it easy for staff to report mistakes without fear. In the U.S., Geisinger Health’s pharmacist-led program boosted medication adherence to 89% for chronic conditions and cut hospital readmissions by 27%. Mayo Clinic used AI to reconcile medications at discharge and cut post-discharge errors by 52%. But in many places, the focus is still on blaming individuals. A 2024 JAMA study found that 89% of medication errors come from system flaws - not human error. A nurse forgets to scan a barcode? Maybe. But why is the system designed so that scanning is an extra step instead of automatic? Why are look-alike drug names still allowed on labels? Why do pharmacists have to manually check 100 prescriptions an hour with no time to talk to patients?The Financial Case Is Clear
Some people say medication safety is too expensive. They’re wrong. Every $1 spent on safety programs returns $7.50 in savings. Pharmacist-led interventions? $13.20 back for every dollar spent. Medicare now ties payments to medication adherence. Plans that hit 90%+ adherence on statins, blood pressure meds, or diabetes drugs get an extra $1.20 to $1.80 per member per month. That’s not charity - it’s smart business. And it’s working. CMS’s 2025 Star Ratings show national adherence rates climbing: 78.4% for cholesterol meds, 76.2% for hypertension, 74.8% for diabetes. The FDA’s new Digital Health Center of Excellence is investing $45 million through 2026 to fund tools that prevent errors. The Drug Supply Chain Security Act requires full electronic tracking of every prescription by November 2025. These aren’t bureaucratic hoops - they’re lifesavers.What Needs to Change
We need three things, right now:- Mandatory national reporting - Right now, only 14% of medication errors in the U.S. are reported. You can’t fix what you don’t measure.
- Standardized training - Only 38 states require pharmacy technicians to be certified. That’s not a national standard - it’s a lottery.
- System-first thinking - Stop blaming nurses and pharmacists. Fix the workflows. Fix the software. Fix the labeling. Fix the communication gaps.
It’s Not About Perfection - It’s About Progress
We won’t eliminate all medication errors overnight. But we can stop pretending they’re unavoidable. The tools exist. The data is clear. The cost of inaction is measured in lives. This isn’t just a hospital issue. It’s a public health emergency. Every pill you take should be safe. Every prescription you get should be clear. Every transition of care should be seamless. If we treat medication safety like the priority it is - not as an afterthought, not as a cost center, but as the foundation of care - we can save hundreds of thousands of lives every year.And that’s not a goal. That’s the bare minimum.
Erin Nemo
December 1, 2025 AT 10:32I’ve seen my grandma mix up her pills after a hospital stay. She thought the blue one was for blood pressure but it was for anxiety. Took her two days to realize. We got lucky she didn’t end up in the ER.
System needs to fix this. Like, yesterday.
ariel nicholas
December 1, 2025 AT 22:04Oh, here we go again-another ‘system failure’ diatribe… while the real problem is that Americans won’t take responsibility for their own health! You want safety? Stop demanding 12 different meds for every little ache! Stop letting Big Pharma dictate your life! We’ve become a nation of chemical zombies-and now you blame the system? Pathetic.
Rachel Stanton
December 2, 2025 AT 21:03Let’s unpack this: medication safety isn’t just about tech or labeling-it’s about care coordination. When discharge instructions aren’t standardized across EHRs, pharmacies, and primary care, you’re setting patients up to fail. We need interoperability mandates-not just ‘voluntary’ compliance.
Also, pharmacist-led medication reconciliation at discharge? That’s not a ‘program,’ it’s a baseline standard. If we treated it like we treat surgical checklists, we’d cut errors by 70% in under a year.
And yes-AI can help, but only if it’s trained on real-world error data, not just clinical trial datasets. Most models don’t account for low-literacy patients or non-English speakers. That’s a design flaw, not a user flaw.
Amber-Lynn Quinata
December 3, 2025 AT 14:38How is this even still a thing?? 😔 I mean, really? People are DYING because doctors can’t write clearly?? And pharmacies are overloaded?? And patients are too scared to ask questions??
It’s not just a system failure-it’s a moral failure. We’re letting people die because we’re too lazy to fix the basics. I’m crying right now. 😭
Someone needs to go to Congress and scream until they listen.
Lauryn Smith
December 5, 2025 AT 13:37I work as a medical assistant. I’ve watched patients stare at their pill bottles like they’re solving a puzzle. One man asked me if the white round pill was his ‘heart medicine’ or his ‘sleep medicine’-he had both. He didn’t know which was which.
We gave him a color-coded chart. He cried. Said he’d never felt so seen.
Simple fixes work. We just have to choose to do them.
Bonnie Youn
December 7, 2025 AT 09:28Y’all are overcomplicating this. Stop blaming systems. Start using apps. There are FREE apps that alert you when to take meds, show you what the pill looks like, and even call your pharmacy if something’s wrong. I use one. My mom uses one. My uncle uses one. We’re not dying.
It’s not about the system. It’s about you. Get with it.
Also-stop letting pharmacists work 100 scripts/hour. They’re humans. Give them breaks. They’re not robots.
Fix the human part first. Tech will follow.
Edward Hyde
December 7, 2025 AT 20:20Medication errors? Nah. That’s just the price of living in a country where people think ‘take one pill’ means ‘take all the pills in the bottle’.
Also, fentanyl pills? That’s not a system failure-that’s a war on drugs failure. Stop legalizing everything and then acting shocked when people OD on fake oxy.
And why are we spending $45M on AI when we can’t even fix the damn barcode scanners? This is performative healthcare.
Charlotte Collins
December 9, 2025 AT 05:16Let’s be brutally honest: the entire U.S. healthcare infrastructure is a Rube Goldberg machine built on paper trails and goodwill. The fact that we’re even debating whether ‘system failure’ is the root cause proves we’re still in denial.
Every time a nurse skips a scan because she’s rushed, it’s not negligence-it’s a design failure. Every time a patient gets confused by five different pill bottles, it’s not confusion-it’s a failure of packaging regulation.
And don’t get me started on how drug names are still allowed to be visually identical. Look-alike, sound-alike. It’s criminal. And nobody’s fired for it.
This isn’t a public health issue. It’s a public betrayal.
Margaret Stearns
December 9, 2025 AT 10:20I’m a retired nurse. I used to fill scripts in the 90s. We had no barcode scanners. No EHR. Just handwritten notes and a lot of phone calls.
Now we have all this tech-but we don’t train people to use it right. I saw a tech give a patient the wrong med because the screen froze. She didn’t know how to check manually.
Training matters more than tools. Always.
And yes-I still write ‘take with food’ in big letters on the bottle. Because some people don’t read the small print.
amit kuamr
December 10, 2025 AT 08:40India has no such problems because we don't overprescribe. One pill for one problem. People take what they need. No fancy apps. No AI. Just common sense and respect for medicine.
Why are Americans so dependent on pills for everything? This is not progress. This is addiction.
Scotia Corley
December 10, 2025 AT 11:25While the emotional appeal of this article is compelling, one must interrogate the underlying assumptions: that systemic inefficiencies are inherently fixable through policy, rather than emergent properties of a fragmented, market-driven healthcare architecture. The $7.50 return on investment metric is statistically misleading without controlling for provider type, patient demographics, and temporal variance. One cannot engineer safety in a system designed for profit maximization.
elizabeth muzichuk
December 10, 2025 AT 21:35My cousin died from a fentanyl pill. He thought it was Percocet. He was 23. He had a job. A dog. A future.
And now? They want to talk about ‘systems’? No. We need to lock up the drug dealers. We need to shut down the dark web pharmacies. We need to make this a CRIME. Not a ‘public health priority.’ A CRIME.
And someone needs to answer for this. Not just ‘the system.’ PEOPLE. REAL PEOPLE. WHO LET THIS HAPPEN.
Debbie Naquin
December 12, 2025 AT 08:47The real question isn’t how to prevent errors-it’s why we still treat medication as a transaction rather than a relationship. A pill isn’t data. It’s a promise. Between doctor and patient. Between pharmacist and community. Between algorithm and life.
When we reduce adherence to a percentage point, we erase the humanity of the act. We forget that taking a pill isn’t just compliance-it’s trust.
Fix the trust. The rest follows.
Karandeep Singh
December 14, 2025 AT 06:12U.S. is just lazy. In my country we just take what doctor says. No apps. No AI. No complaints. Simple. Why make it hard?