Adverse Drug Events: What They Are and How to Stay Safe
When you take a medication, you expect it to help—not hurt. But adverse drug events, harmful and unintended reactions to medicines. Also known as drug reactions, they can range from a mild rash to life-threatening organ failure. These aren’t just rare accidents. Every year, millions of people in the U.S. end up in the hospital because of them. And the scary part? Many of these events happen because of things you can control.
Drug interactions, when two or more medications clash in your body are one of the biggest culprits. Take a common painkiller like ibuprofen with a blood thinner, and you could bleed internally. Or mix an old-school antihistamine like Benadryl with a sleep aid, and you might increase your risk of dementia over time. Then there’s side effects, predictable reactions tied to how a drug works—like nausea from chemo or dizziness from blood pressure meds. These aren’t always dangerous, but they can make you quit your medicine, which is worse than the side effect itself.
Some reactions are unpredictable. That’s the silent killer. You could take a drug you’ve used for years, and suddenly your liver shuts down or your skin starts peeling. These are called Type B reactions, rare, severe, and not linked to the drug’s main action. They’re hard to plan for, but knowing your own body helps. If you’ve had strange reactions before—rashes, swelling, sudden fatigue—write them down. Tell every doctor. Update your EHR records. That’s how you stop the next one.
And it’s not just about what’s in your pill bottle. Over-the-counter drugs, herbal supplements, even grapefruit juice can turn a safe dose into a dangerous one. A simple allergy list update can prevent a deadly reaction. A pill organizer keeps you from double-dosing. Talking to your pharmacist about cash prices isn’t just about saving money—it’s about sticking to your meds so you don’t end up in the ER because you skipped doses.
Adverse drug events don’t happen in a vacuum. They’re tied to how you take your medicine, what else you’re on, your age, your liver and kidney health, even your sleep schedule. That’s why the posts here cover everything from MAOIs and dietary restrictions to how cold urticaria can mimic a drug reaction, and why certain antibiotics are safer during pregnancy. You’ll find real advice on tracking your meds, spotting hidden hypertension from NSAIDs, and understanding why some generics can’t be swapped without checking FDA codes.
This isn’t about scaring you off medicine. It’s about making sure you’re in control. The right drug at the right dose can save your life. But without awareness, even the safest treatment can turn dangerous. Below, you’ll find practical guides that help you ask the right questions, spot red flags early, and work with your care team—not just take pills and hope for the best.
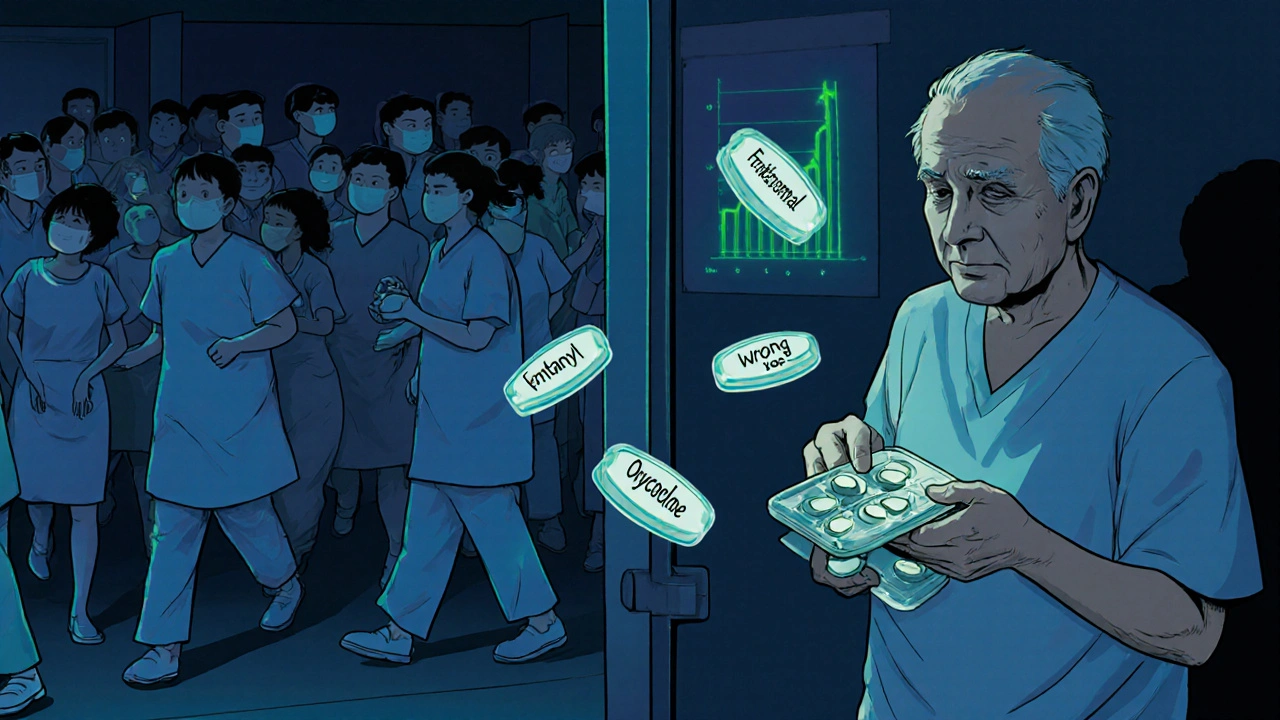
Why Medication Safety Is a Public Health Priority in Healthcare
Medication errors cause over 1.5 million ER visits annually in the U.S. alone. This article explains why medication safety is a critical public health priority, backed by data on costs, deaths, and proven solutions.