Antihistamines: What They Are, How They Work, and What You Need to Know
When your nose runs, your eyes itch, or your skin breaks out in hives, it’s usually because your body is overreacting to something harmless. That’s where antihistamines, drugs that block histamine, a chemical your body releases during allergic reactions. Also known as allergy pills, they’re one of the most common over-the-counter treatments for stuffy noses, sneezing, and itchy skin. Unlike antibiotics, they don’t fight germs—they calm your immune system’s false alarms. You’ve probably seen them in the pharmacy aisle: loratadine, cetirizine, diphenhydramine. But not all antihistamines are the same, and using the wrong one can leave you drowsy, dry-mouthed, or worse.
Antihistamines work by stopping histamine from binding to receptors in your body. Histamine is what causes swelling, redness, and itching during an allergic response. If you get hives after stepping into cold air—like in cold urticaria, a condition where cold triggers hives and itching—antihistamines are often the first line of defense. Same goes for seasonal allergies, insect bites, or even reactions to certain foods. But they’re not just for allergies. Some are used off-label for motion sickness, sleep issues, or even nausea. The key is matching the right type to your symptom. First-generation ones like diphenhydramine cross into your brain and make you sleepy. Second-generation ones like loratadine mostly stay in your bloodstream, so you can drive, work, or study without crashing.
Not every reaction responds the same. If you have chronic hives that won’t go away, or if your allergies flare up even after taking antihistamines daily, you might need something stronger. That’s where doctors consider other options—like adding a steroid, switching to a different class of drug, or testing for underlying conditions. Some people don’t realize their hives are tied to cold exposure, stress, or even certain medications. And if you’re on other drugs—like antidepressants or blood pressure meds—antihistamines can interact in ways you wouldn’t expect. That’s why it’s not just about popping a pill. It’s about understanding your body’s signals and knowing when to stop self-treating and see a professional.
Looking at the posts here, you’ll find real stories about how antihistamines fit into bigger health pictures—from managing cold-induced hives to avoiding dangerous drug combos. You’ll see which ones work best for sleep, which ones cause dryness, and why some people need higher doses than others. There’s no one-size-fits-all solution. But with the right info, you can pick the one that actually helps—without the side effects you didn’t sign up for.
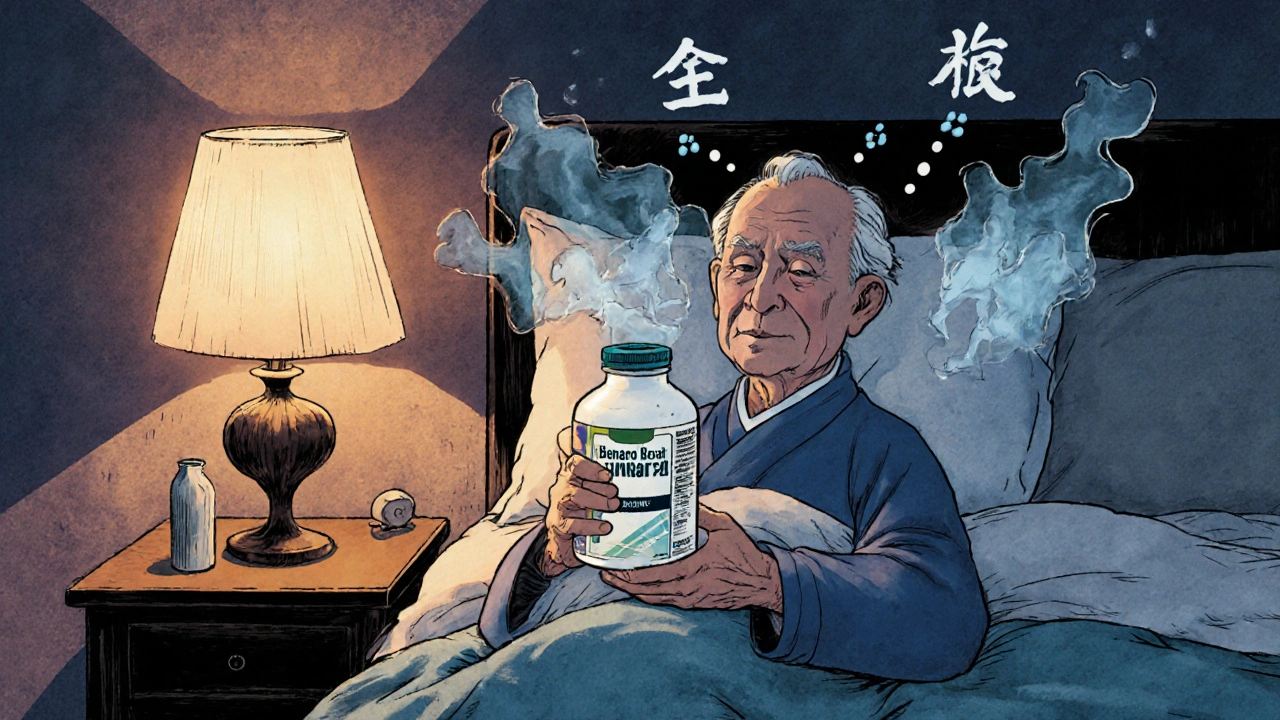
Antihistamines and Dementia Risk: What You Need to Know About Long-Term Use
First-generation antihistamines like Benadryl may increase dementia risk in older adults due to anticholinergic effects. Learn which ones to avoid, safer alternatives, and what the latest research really says.