Back Pain Medications: What Works, What Doesn't, and What to Avoid
When you're dealing with back pain medications, drugs used to reduce pain and inflammation in the lower or upper spine. Also known as analgesics for spinal discomfort, these are among the most commonly prescribed treatments for chronic or acute back issues. But not all of them are created equal—and some can do more harm than good if used without understanding how they work.
Most people start with NSAIDs, nonsteroidal anti-inflammatory drugs like ibuprofen or naproxen that reduce swelling and nerve irritation. They help a lot for short-term flare-ups, especially when the pain comes from a strained muscle or inflamed joint. But long-term use? That’s where things get risky. Studies show regular NSAID use can lead to stomach ulcers, kidney damage, and even higher blood pressure. And if you’ve got kidney disease or heart problems, they might not be safe at all.
Then there are muscle relaxants, medications like cyclobenzaprine or methocarbamol that calm overactive muscles causing spasms. They work fast, often giving relief within hours. But they make you drowsy—sometimes so much that driving or operating machinery becomes dangerous. And they don’t fix the root cause. If your back pain comes from a herniated disc or spinal stenosis, muscle relaxants just mask the symptoms. They’re a temporary bandage, not a cure.
Many still turn to opioids, strong painkillers like oxycodone or hydrocodone that act on brain receptors to dull pain signals. But the data is clear: for most back pain, opioids offer little long-term benefit and carry a high risk of dependence. The CDC and major medical groups now warn against using them for routine back pain. If you’ve been on them for more than a few weeks, talk to your doctor about tapering off—there are safer, more sustainable options.
What’s often overlooked? Back pain medications aren’t the whole story. The most effective plans combine them with movement, physical therapy, and posture changes. A pill won’t fix a weak core or a desk job that’s wrecking your spine. But used wisely, the right medication can give you enough relief to start moving again—and movement is what actually heals.
You’ll find posts here that break down exactly which drugs show up in real-world studies, which ones doctors quietly avoid, and how to spot the difference between a helpful treatment and a dangerous shortcut. From comparing over-the-counter options to understanding why some prescriptions come with hidden red flags, this collection gives you the facts you need to make smarter choices—without the hype.
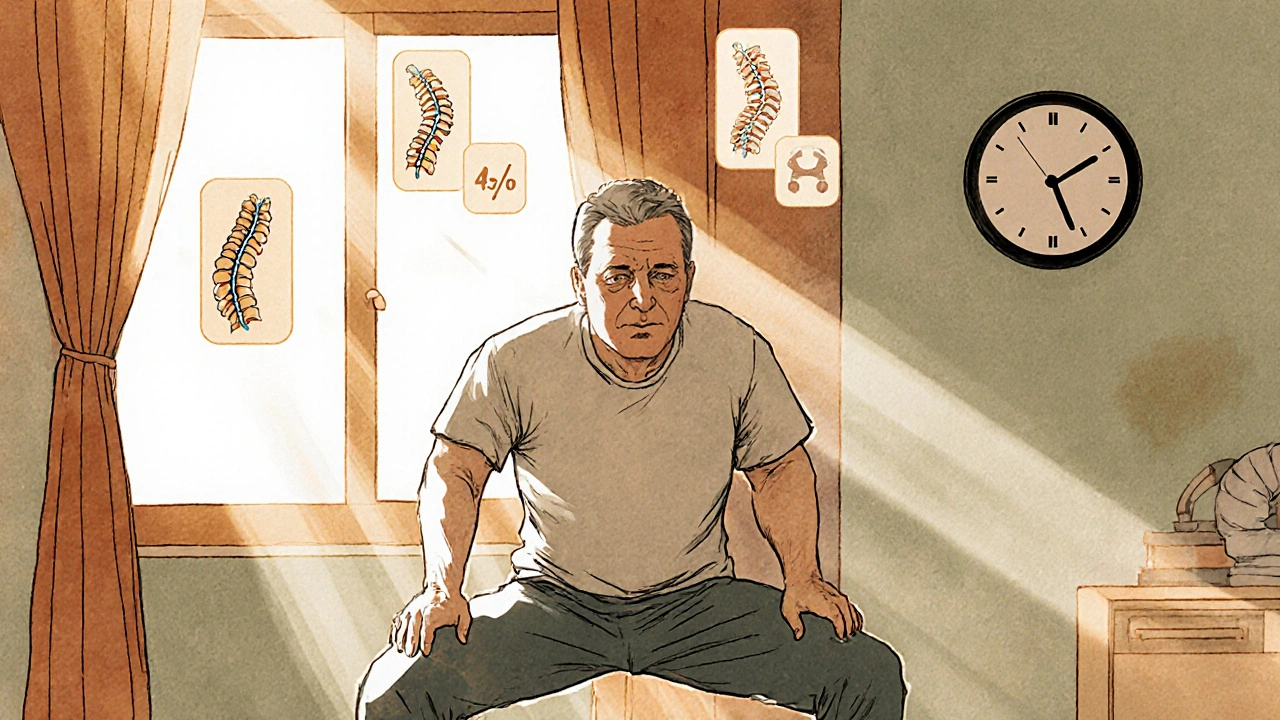
Chronic Back Pain: Physical Therapy, Medications, and Self-Management That Actually Work
Chronic back pain lasting more than 12 weeks requires more than quick fixes. Learn how physical therapy, smart medication use, and daily self-management can reduce pain and restore function - backed by science and real patient results.