Corticosteroid Hyperglycemia: How Steroids Raise Blood Sugar and What to Do
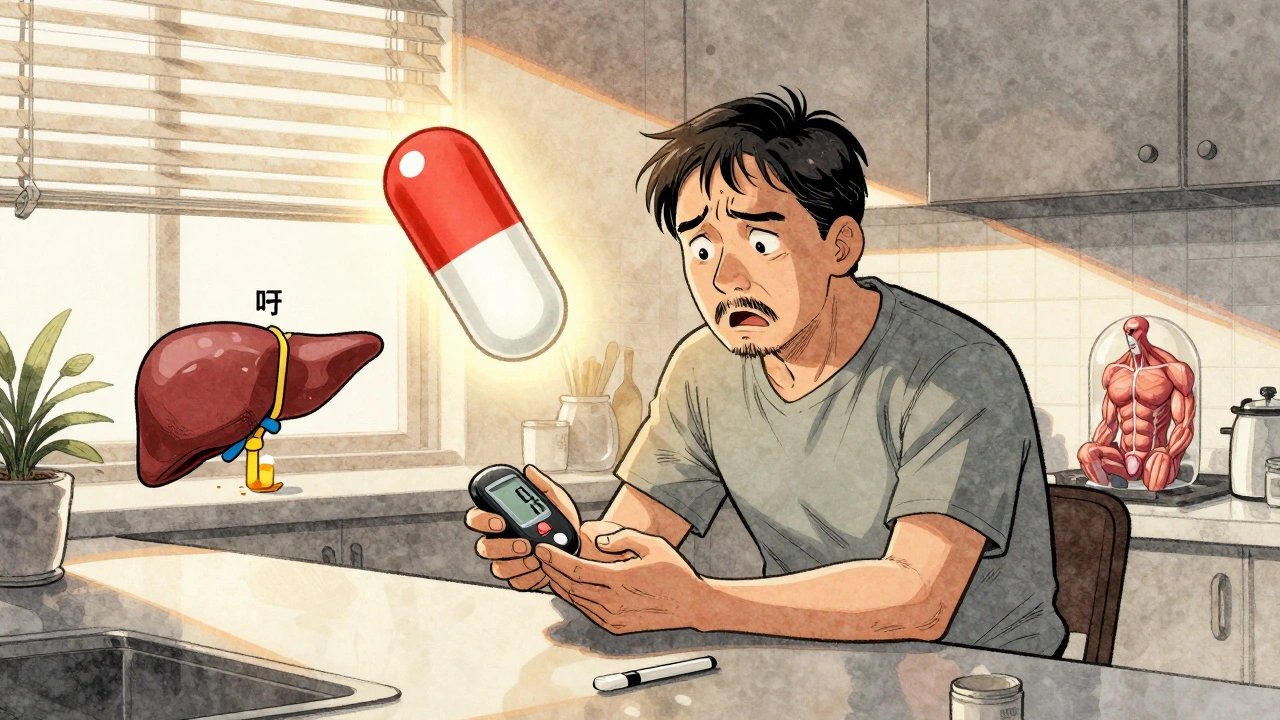
When you take corticosteroid hyperglycemia, a condition where steroid medications cause elevated blood sugar levels. Also known as steroid-induced diabetes, it’s not a true diabetes diagnosis—it’s a temporary metabolic shift triggered by drugs like prednisone, dexamethasone, or methylprednisolone. These medications are powerful anti-inflammatories used for asthma, rheumatoid arthritis, lupus, and even severe allergies. But for many people, especially those with pre-existing insulin resistance or a family history of diabetes, they turn blood sugar into a rollercoaster.
Corticosteroids, a class of synthetic hormones mimicking cortisol, the body’s natural stress hormone work by telling the liver to release more glucose into the bloodstream. At the same time, they make muscle and fat cells less responsive to insulin—the hormone that normally pulls sugar out of the blood. The result? Sugar piles up. This isn’t rare. Studies show up to 50% of people on long-term oral steroids develop elevated glucose levels, and about 1 in 10 end up needing treatment for it. Even short courses, like a 5-day prednisone pack, can cause noticeable spikes in fasting glucose.
It’s not just about the dose. Risk goes up with age, weight, and a history of prediabetes. People taking more than 20 mg of prednisone daily for over a week are most likely to see trouble. But even low doses can push someone over the edge if their body is already struggling to manage sugar. And here’s the catch: many don’t feel it. No thirst, no frequent urination—just a weirdly high reading on a routine blood test. That’s why doctors check fasting glucose before starting long-term steroid therapy and again after a few weeks.
Managing this isn’t about stopping the steroids. Often, you can’t. Instead, it’s about working with your doctor to monitor, adjust, and protect. Some people need metformin or insulin temporarily. Others just need to eat fewer carbs, move more, and check their sugar a few times a week. The goal isn’t to eliminate steroids—it’s to keep sugar from doing damage while you’re on them. High blood sugar for weeks can hurt nerves, kidneys, and eyes. That’s why catching it early matters.
You’ll find real-world advice here on how to track sugar changes, which foods help or hurt, how to talk to your doctor about alternatives, and what to do if you’re on steroids for a flare-up and your glucose spikes. We also cover how this interacts with other meds, like diuretics or NSAIDs, that can make things worse. This isn’t theoretical. These posts come from people who’ve lived it—patients, nurses, and clinicians who’ve seen the numbers climb and figured out how to bring them back down.
Corticosteroid-Induced Hyperglycemia and Diabetes: How to Monitor and Manage It
Corticosteroid-induced hyperglycemia is a common and dangerous side effect of steroid therapy. Learn how to monitor blood sugar, when to start insulin, and how to prevent complications in both hospital and home settings.