Dementia Risk: What Actually Increases It and How to Reduce It
When we talk about dementia risk, the likelihood of developing cognitive decline that interferes with daily life. Also known as neurodegenerative risk, it’s not just about getting older—it’s about what happens inside your brain over time. Many people assume dementia is inevitable with age, but that’s not true. Studies show nearly 40% of dementia cases could be prevented or delayed by managing lifestyle and medical factors.
One major hidden driver of dementia risk, the likelihood of developing cognitive decline that interferes with daily life. Also known as neurodegenerative risk, it’s not just about getting older—it’s about what happens inside your brain over time. is poor blood flow to the brain. Conditions like high blood pressure, kidney disease, and liver problems don’t just affect those organs—they silently starve your neurons. That’s why managing medications like anticoagulation, the use of drugs to prevent blood clots that can block brain vessels. Also known as blood thinning therapy, it’s critical for people with heart or vascular issues. isn’t just about preventing strokes. It’s about keeping your brain oxygenated. Similarly, medication-induced hypertension, high blood pressure caused by common drugs like NSAIDs, steroids, or decongestants. Also known as drug-induced high BP, it’s often overlooked but directly linked to faster cognitive decline. can quietly raise your risk without you noticing.
Then there’s the brain chemistry side. Some antidepressants and sedatives, like MAOIs, powerful antidepressants that alter brain chemicals but require strict dietary controls. Also known as monoamine oxidase inhibitors, they’re effective but carry long-term neurological trade-offs. or benzodiazepines, sedatives often prescribed for anxiety or sleep but linked to memory problems with long-term use. Also known as benzos, they’re not harmless, even if your doctor says they’re safe., can interfere with how your brain processes and stores information. Long-term use doesn’t just make you drowsy—it may accelerate the path toward dementia risk. Even thyroid imbalances, like those seen in sick euthyroid syndrome, a temporary disruption of thyroid hormone levels during illness that mimics hypothyroidism. Also known as NTIS or low T3 syndrome, it’s often misdiagnosed but affects brain metabolism., can cloud thinking if left unaddressed.
And it’s not just drugs. Sleep matters. If you’re fighting circadian rhythm disorders, conditions like jet lag or delayed sleep phase that throw off your natural sleep-wake cycle. Also known as sleep phase disorders, they disrupt the brain’s nightly cleanup process., your brain doesn’t get the chance to flush out toxic proteins linked to Alzheimer’s. Same with chronic inflammation from untreated conditions like ulcers or gallbladder disease—those don’t just hurt your gut, they trigger brain inflammation over time.
What you’ll find here isn’t guesswork. Every article below comes from real clinical data, patient experiences, and updated guidelines. You’ll see how generic meds cut long-term costs that otherwise lead to poor adherence and worse outcomes. You’ll learn which drugs are safe in pregnancy, how to avoid dangerous combos like opioids and benzos, and why a simple 90-day prescription refill can make a bigger difference than you think. This isn’t about fear—it’s about control. You can’t change your age, but you can change your habits, your meds, and your environment. Let’s look at what actually works.
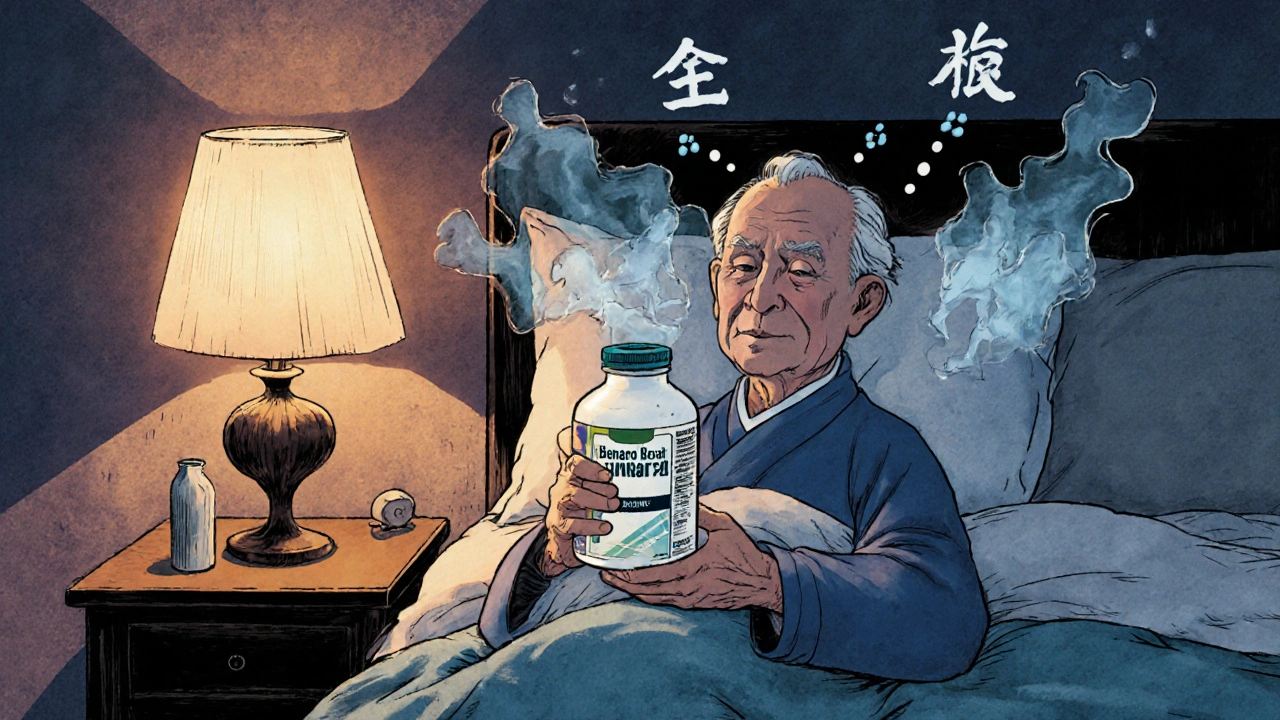
Antihistamines and Dementia Risk: What You Need to Know About Long-Term Use
First-generation antihistamines like Benadryl may increase dementia risk in older adults due to anticholinergic effects. Learn which ones to avoid, safer alternatives, and what the latest research really says.