Generic Drug Approval: What It Really Means and How It Affects Your Prescription
When you pick up a prescription and see a different name on the bottle than what your doctor wrote, it’s not a mistake—it’s generic drug approval, the process the FDA uses to confirm that a generic version of a brand-name drug is just as safe and effective. Also known as FDA generic approval, this system lets millions of people save money without sacrificing results. The FDA doesn’t just accept claims—it tests every single generic to prove it delivers the same active ingredient, in the same amount, at the same speed as the original. This isn’t guesswork. It’s science.
But not all generics are created equal. The therapeutic equivalency, a rating system the FDA uses to classify whether a generic can be automatically swapped for a brand-name drug. Also known as TE codes, it’s printed in the Orange Book and tells pharmacists exactly which substitutions are allowed. Some drugs have a code that means they’re interchangeable—like most antibiotics or blood pressure pills. Others don’t. Why? Because for drugs with a narrow therapeutic index—like warfarin, thyroid meds, or seizure drugs—even tiny differences in absorption can cause harm. That’s why your pharmacist can’t just swap them without checking with your doctor.
And here’s the thing: generic substitution, the practice of replacing a brand-name drug with a generic at the pharmacy counter. Also known as pharmaceutical substitution, it’s legal in every state—but rules vary. Some states let pharmacists substitute by default. Others require your permission. Some won’t substitute at all for certain drugs. That’s why you should always ask: "Is this the generic version? Can I get the brand if I want?" It’s your right to know. And if you’re on a chronic condition like diabetes or heart disease, switching generics between refills can sometimes cause unexpected side effects—even if both are "approved." That’s because different manufacturers use different fillers and coatings, which can change how the drug dissolves in your body.
Behind every approved generic is a mountain of data: dissolution tests, bioequivalence studies, manufacturing audits. The FDA inspects foreign factories just like U.S. ones. A generic made in India or China has to meet the same standards as the brand made in New Jersey. That’s why a $5 generic for metformin works just as well as the $150 brand. But it’s also why you should never assume all generics are identical. If you notice a change in how you feel after a refill switch, tell your doctor. It’s not in your head—it could be the filler.
What you’ll find below are real-world stories and clear explanations about how generic drug approval affects your daily life. From how TE codes block certain swaps, to why your insulin might behave differently after a manufacturer change, to how pharmacies use discount tools to find the cheapest generic—these posts cut through the noise. You’ll learn what to ask, what to watch for, and when to push back. No jargon. No fluff. Just what matters when your health is on the line.
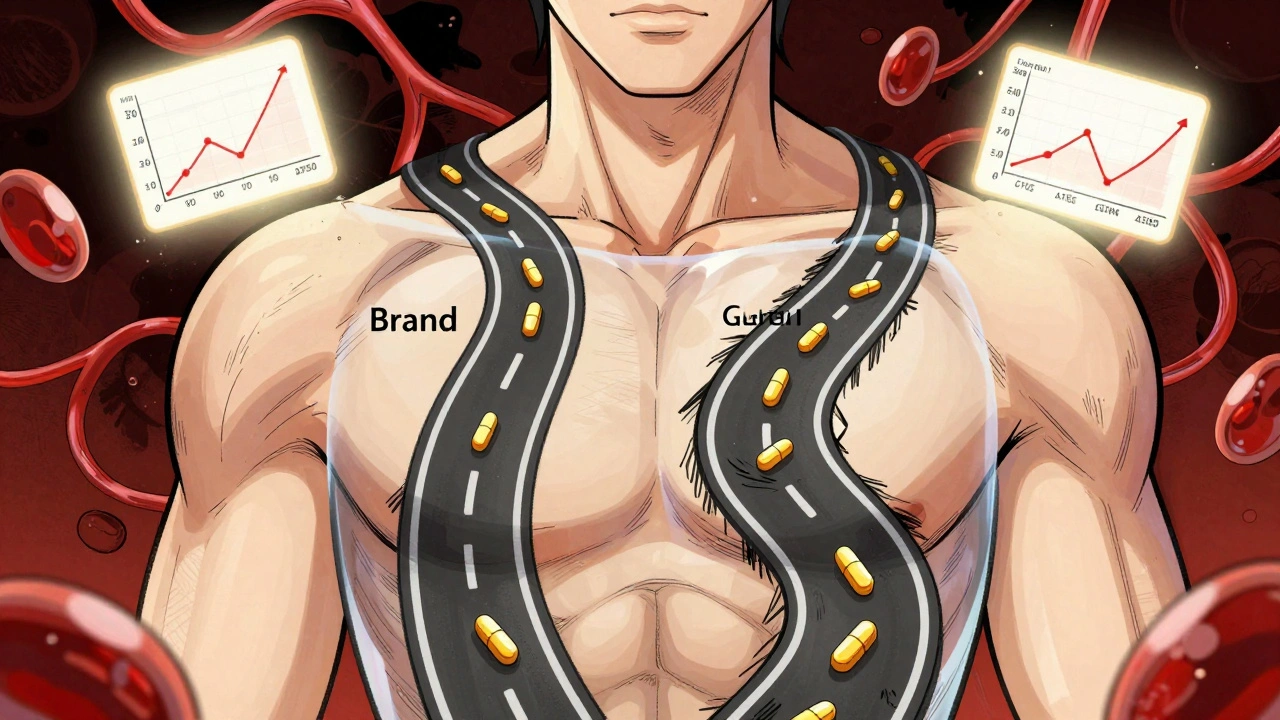
Bioequivalence Explained: FDA Requirements to Prove Generic Drug Equivalence
Bioequivalence is how the FDA ensures generic drugs work just like brand-name versions. It's proven through strict pharmacokinetic studies measuring Cmax and AUC, with a 90% confidence interval between 80% and 125%. This science keeps generics safe, effective, and affordable.