Infliximab: What It Is, How It Works, and What You Need to Know
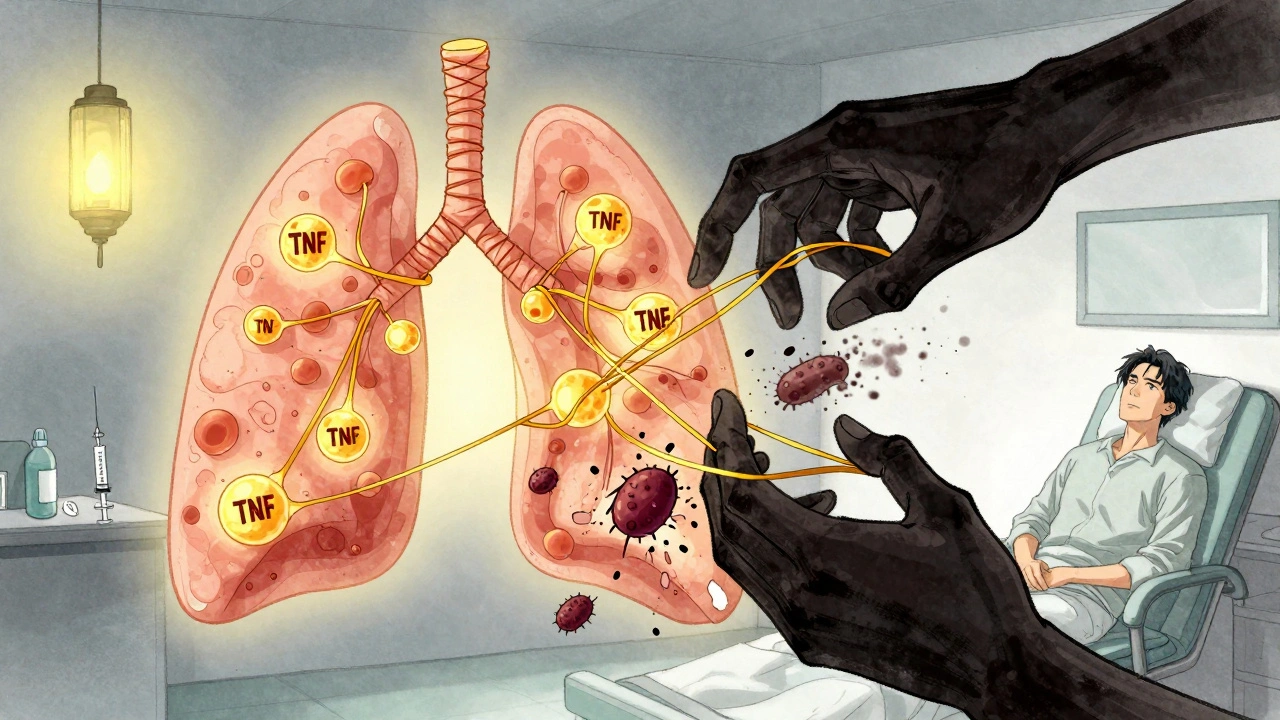
When your immune system turns against your own body, infliximab, a biologic drug that blocks tumor necrosis factor (TNF), a key driver of inflammation in autoimmune diseases. Also known as a TNF inhibitor, it stops the body’s overactive immune response before it damages joints, the gut, or other tissues. Unlike painkillers or steroids that just mask symptoms, infliximab targets the root cause — the overproduction of TNF-alpha, a protein that triggers swelling, pain, and tissue destruction in conditions like rheumatoid arthritis, Crohn’s disease, and psoriasis.
It’s not a pill. You get infliximab through an IV infusion, usually every 4 to 8 weeks, in a clinic or hospital. That’s because it’s a large protein molecule made from living cells — a biologic drug, a type of medication derived from living organisms that targets specific parts of the immune system. This makes it powerful but also more complex than traditional drugs. It doesn’t work for everyone, and some people develop antibodies against it over time, reducing its effectiveness. That’s why doctors often combine it with methotrexate — to help the body accept it longer and boost results.
Because it suppresses part of your immune system, you’re more vulnerable to infections. Before starting, you’ll be tested for tuberculosis and hepatitis. If you’ve had cancer or heart failure, infliximab may not be safe for you. It’s not a first-line treatment — it’s for when other drugs fail. But for many, it’s life-changing. People with severe Crohn’s who couldn’t eat without pain have returned to normal meals. Others with joint damage from rheumatoid arthritis have walked without crutches again. The science behind it is solid: clinical trials show it reduces inflammation markers, heals intestinal lining in Crohn’s, and slows joint erosion in arthritis.
There are other TNF inhibitors, a class of biologic drugs that block the same inflammatory pathway as infliximab — like adalimumab or etanercept — but infliximab was one of the first, and it’s still widely used. Each has slight differences in dosing, delivery, and side effect profiles. Some people respond better to one than another. If infliximab stops working, switching to another TNF inhibitor or a different class of biologic might help.
What you’ll find in the posts below isn’t just about infliximab itself. It’s about the bigger picture: how biologics fit into long-term disease management, what to watch for with side effects, how to handle missed doses, and why medication safety matters when your immune system is on pause. You’ll see how people manage life on these drugs — from travel tips for keeping meds stable to understanding how other conditions like diabetes or liver disease affect treatment choices. This isn’t a textbook. It’s real-world guidance from people who’ve been there, and doctors who’ve seen what works.
TNF Inhibitors and TB Reactivation: Screening and Monitoring Guidelines
TNF inhibitors effectively treat autoimmune diseases but carry a risk of reactivating latent tuberculosis. Screening with TST or IGRA, treating latent TB before starting therapy, and ongoing symptom monitoring are essential to prevent life-threatening complications.