Insulin for Steroid Hyperglycemia: What You Need to Know
When someone takes steroids, powerful anti-inflammatory drugs like prednisone or methylprednisolone used for autoimmune diseases, asthma, or after organ transplants, their blood sugar can spike—sometimes dangerously so. This isn’t diabetes in the classic sense, but it’s real, measurable hyperglycemia, abnormally high blood glucose levels that can lead to dehydration, nerve damage, and long-term complications if ignored. For many, the only reliable fix is insulin, a hormone the body normally makes to move sugar from blood into cells. Unlike oral meds, insulin works fast and directly, making it the go-to when steroids are necessary but blood sugar won’t calm down.
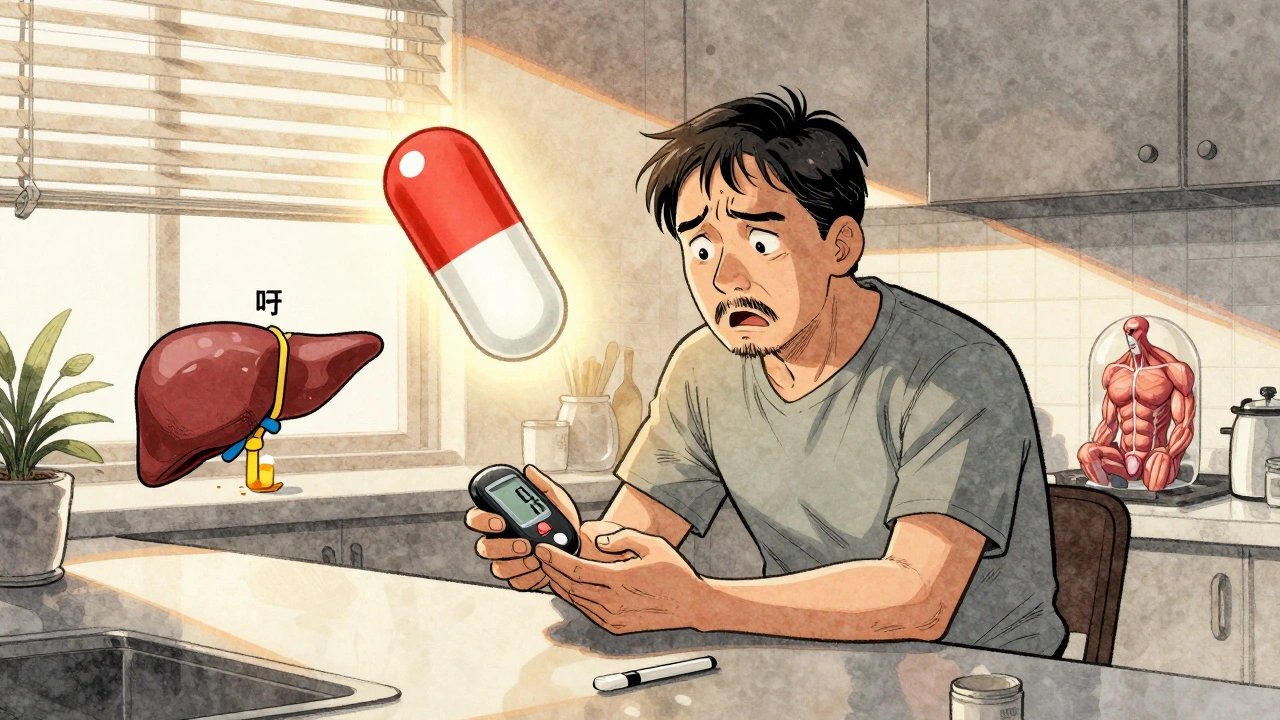
Steroid hyperglycemia doesn’t happen to everyone, but it’s common in people on high doses for more than a few days. It’s not about being "pre-diabetic"—it’s about how steroids mess with liver sugar production and block insulin’s ability to do its job. That’s why even people with no prior diabetes history can end up needing insulin. Doctors don’t just slap on a pill; they watch glucose levels closely, often starting with basal insulin at night to handle fasting spikes, then adding quick-acting insulin before meals if post-meal numbers stay high. It’s not permanent. Once steroids are tapered down, many people can stop insulin entirely. But until then, skipping it isn’t an option—high sugars during steroid treatment can delay healing, increase infection risk, and even lead to diabetic ketoacidosis in severe cases.
What you won’t find in most guides is how often this is misunderstood. Some patients think they’re now "diabetic for life" because they needed insulin during steroid treatment. Others delay treatment because they fear needles or think diet alone will fix it. Neither is true. This is a temporary, drug-induced metabolic shift—and insulin is the most precise tool to manage it. The same goes for people on long-term steroids for conditions like rheumatoid arthritis or COPD. They don’t need to suffer through high sugars. Insulin can be adjusted week to week as steroid doses change, and it’s safer than trying to force oral meds that weren’t designed for this kind of spike.
Below, you’ll find real-world guidance on how insulin is used in this setting, how to monitor progress, and what other treatments might help—without replacing insulin when it’s truly needed. These aren’t theory pieces. They’re practical, tested approaches from patients and providers who’ve walked this path.
Corticosteroid-Induced Hyperglycemia and Diabetes: How to Monitor and Manage It
Corticosteroid-induced hyperglycemia is a common and dangerous side effect of steroid therapy. Learn how to monitor blood sugar, when to start insulin, and how to prevent complications in both hospital and home settings.