Steroid Diabetes Care: Managing Blood Sugar When Taking Steroids
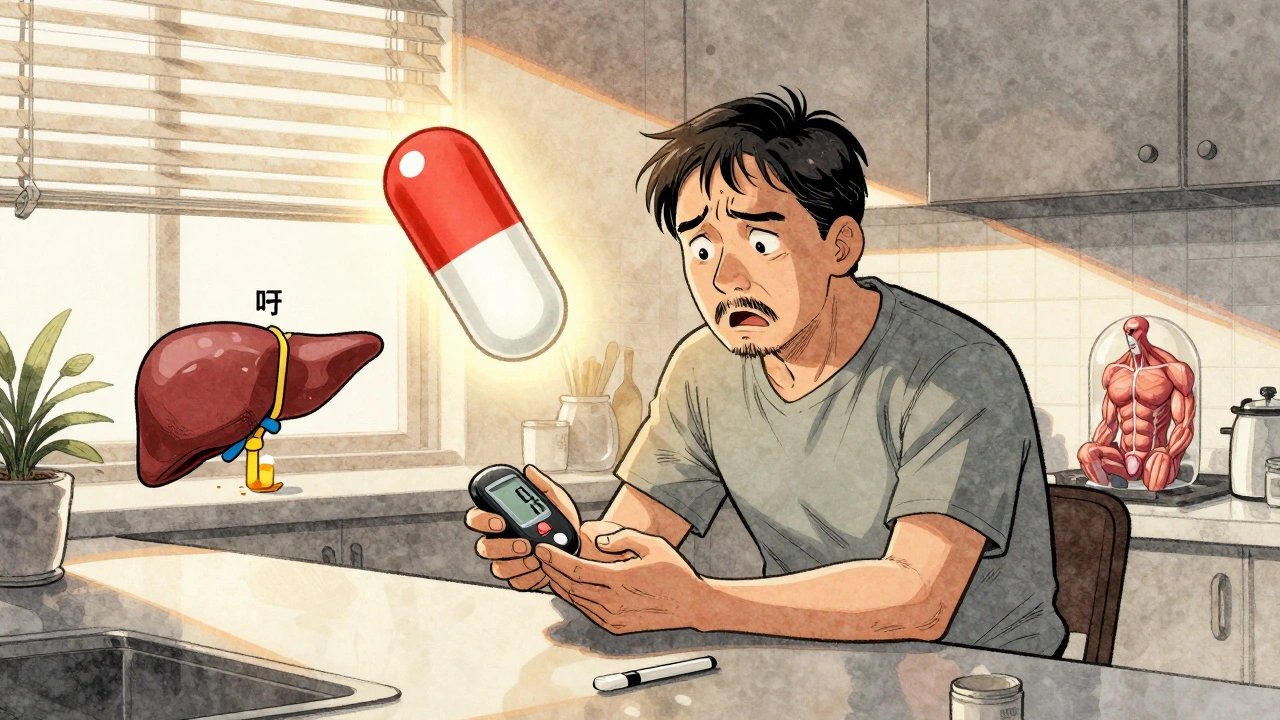
When you take steroids, powerful anti-inflammatory drugs like prednisone or dexamethasone used for autoimmune diseases, asthma, or after organ transplants. Also known as corticosteroids, they can sharply raise blood sugar—even in people who’ve never had diabetes before. This isn’t a side effect you can ignore. It’s called steroid-induced diabetes, a temporary but serious condition where steroid use triggers high blood glucose levels. Unlike type 2 diabetes, it often shows up fast, sometimes within days of starting the medication, and it doesn’t always go away when you stop the steroids.
People on long-term steroids—especially those over 40, overweight, or with a family history of diabetes—are at highest risk. But even healthy adults can see their fasting glucose jump from 90 to 180 mg/dL after just a week of prednisone. The problem? Steroids make your liver pump out more glucose and block insulin from doing its job. Your body ends up swimming in sugar, even if you eat normally. Left unchecked, this can lead to dehydration, nerve damage, or even diabetic ketoacidosis. The goal isn’t to avoid steroids when they’re medically needed. It’s to manage the blood sugar they cause.
Good steroid diabetes care, a targeted approach to controlling glucose levels during steroid therapy means more than just checking your sugar. It means knowing when to test (before meals and 2 hours after), understanding how dose timing affects peaks, and adjusting food or meds accordingly. Some people need oral drugs like metformin. Others need insulin, even if just for a few weeks. Your doctor might lower your steroid dose if possible, or switch to a different type. But you can’t wait for symptoms to get bad. That’s why tracking is key—just like with any diabetes, you need data to make smart choices.
What you’ll find below are real, practical guides on how to handle this. From daily blood sugar checks that actually work, to how to talk to your pharmacist about medication timing, to what foods help stabilize glucose when steroids are in your system. These aren’t theory pieces. They’re tools built from patient experiences and clinical practice. Whether you’re on a short steroid course or managing long-term treatment, the advice here is meant to keep you safe, in control, and out of the hospital.
Corticosteroid-Induced Hyperglycemia and Diabetes: How to Monitor and Manage It
Corticosteroid-induced hyperglycemia is a common and dangerous side effect of steroid therapy. Learn how to monitor blood sugar, when to start insulin, and how to prevent complications in both hospital and home settings.