Steroid-Induced Diabetes: Causes, Risks, and How to Manage It
When you take steroid-induced diabetes, a form of high blood sugar triggered by corticosteroid medications. Also known as glucocorticoid-induced hyperglycemia, it’s not the same as type 1 or type 2 diabetes—it’s a temporary metabolic shift caused by drugs meant to reduce inflammation. This isn’t rare. People on long-term prednisone, dexamethasone, or other corticosteroids for asthma, arthritis, or autoimmune diseases often see their blood sugar climb—even if they’ve never had diabetes before.
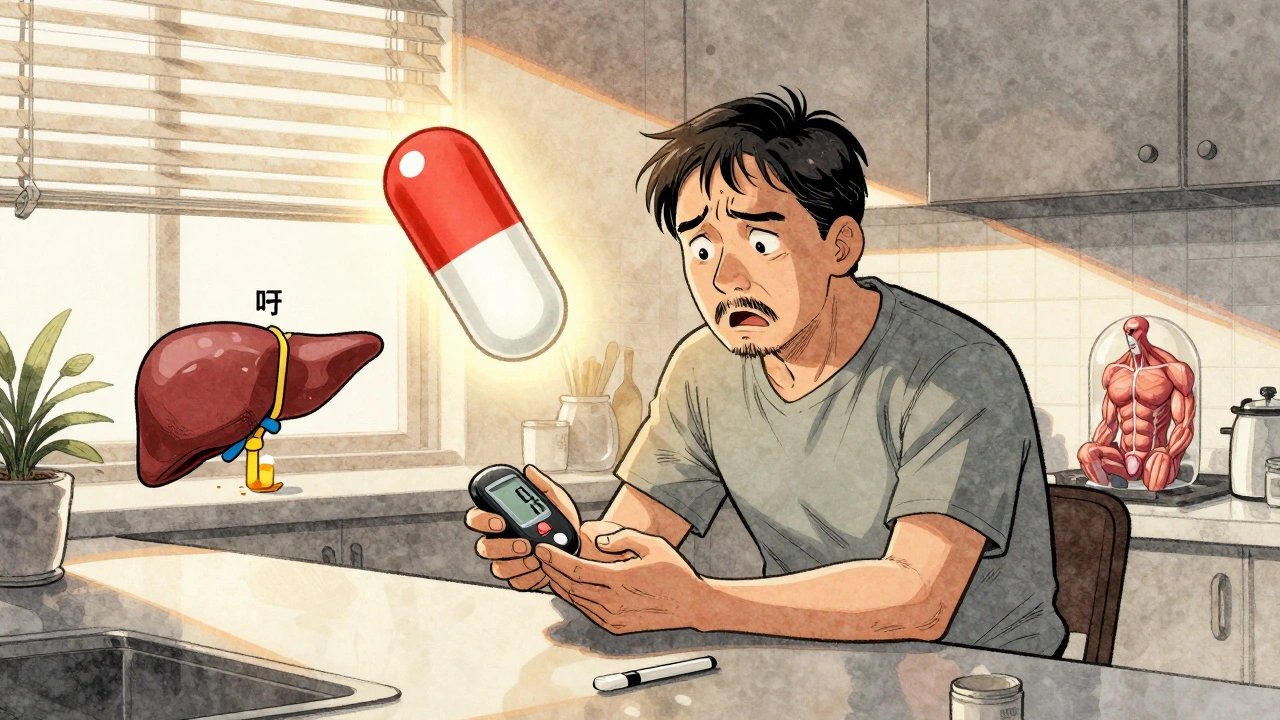
Why does this happen? Corticosteroids mess with how your body uses insulin. They make your liver pump out more glucose, and they block insulin from doing its job in muscles and fat cells. The result? Sugar builds up in your blood. It’s not your fault. It’s not because you ate too much sugar. It’s a direct side effect of the medication. And it’s more likely if you’re overweight, over 45, have a family history of diabetes, or already have prediabetes. Studies show up to 30% of people on daily steroids for more than a month develop elevated blood sugar.
Managing this isn’t about stopping the steroids—often, those drugs are life-saving. It’s about monitoring and adjusting. Blood sugar checks become part of your routine. Some people need oral meds like metformin; others need insulin, even short-term. The key is catching it early. Symptoms like extreme thirst, frequent urination, or blurry vision shouldn’t be ignored. Your doctor can adjust your steroid dose, suggest dietary tweaks, or recommend activity changes to help your body handle the extra sugar. This isn’t a permanent condition for most, but it can become one if left unchecked.
Related to this are the risks of corticosteroids, powerful anti-inflammatory drugs commonly prescribed for chronic conditions. They help with flare-ups, but they also raise blood pressure, weaken bones, and can cause weight gain—all of which make blood sugar harder to control. Then there’s diabetes management, the daily actions needed to keep blood sugar in a safe range. It’s not just pills or shots. It’s knowing which foods spike sugar, how exercise lowers it, and when to test. The posts below cover real-world ways to handle these challenges: from foot care to medication safety, from tracking tools to understanding drug interactions. You’ll find practical advice from people who’ve been there—not theory, but what works in daily life.
Corticosteroid-Induced Hyperglycemia and Diabetes: How to Monitor and Manage It
Corticosteroid-induced hyperglycemia is a common and dangerous side effect of steroid therapy. Learn how to monitor blood sugar, when to start insulin, and how to prevent complications in both hospital and home settings.