TB Reactivation: What You Need to Know About Latent Tuberculosis Coming Back
When TB reactivation, the process where dormant tuberculosis bacteria become active again and cause disease. Also known as reactivated tuberculosis, it’s not a new infection—it’s the same bacteria that stayed hidden for months or years, then woke up. Most people who catch TB never get sick right away. Their immune system walls off the bacteria in the lungs, creating what’s called latent tuberculosis, a silent, non-contagious form of TB where the bacteria are alive but inactive. That’s fine—until something weakens the body’s defenses. Then, those hidden germs can multiply, spread, and turn into active TB disease. That’s TB reactivation.
TB reactivation doesn’t happen randomly. It’s tied to things that stress your immune system. Diabetes, a condition that impairs immune response and increases infection risk. People with diabetes are 2 to 3 times more likely to reactivate TB. Corticosteroids, powerful anti-inflammatory drugs that suppress immune function. Long-term steroid use, whether for asthma, arthritis, or autoimmune diseases, quietly lowers your body’s ability to keep TB in check. Even kidney disease, a condition that reduces immune cell activity and alters drug metabolism. can tip the balance. If you’ve had TB in the past—or even just a positive skin or blood test for it—and you’re now on steroids, have diabetes, or are on dialysis, you’re in a high-risk group.
TB reactivation doesn’t always come with a sudden fever or cough. Sometimes it starts slow: unexplained weight loss, night sweats that soak your sheets, tiredness that won’t go away, or a cough that lingers past a cold. These aren’t just signs of aging or stress—they’re red flags. The bacteria usually attack the lungs, but they can spread to bones, kidneys, or the brain. That’s why early detection matters. A chest X-ray and sputum test can confirm if TB has come back. Treatment isn’t simple. It takes at least six months of multiple antibiotics. Skipping doses or stopping early? That’s how drug-resistant TB forms. And once you have that, treatment becomes longer, costlier, and harder to manage.
What you’ll find below are real, practical guides from people who’ve lived through this. You’ll see how to spot early warning signs before it turns serious. You’ll learn how diabetes and steroid use connect to TB reactivation—not just in theory, but in daily life. You’ll find out how to stay on track with meds when you’re juggling multiple prescriptions. And you’ll see how simple steps like checking your symptoms monthly or talking to your pharmacist about drug interactions can make all the difference. This isn’t about fear. It’s about knowing what to watch for, when to act, and how to protect yourself when your body’s defenses are down.
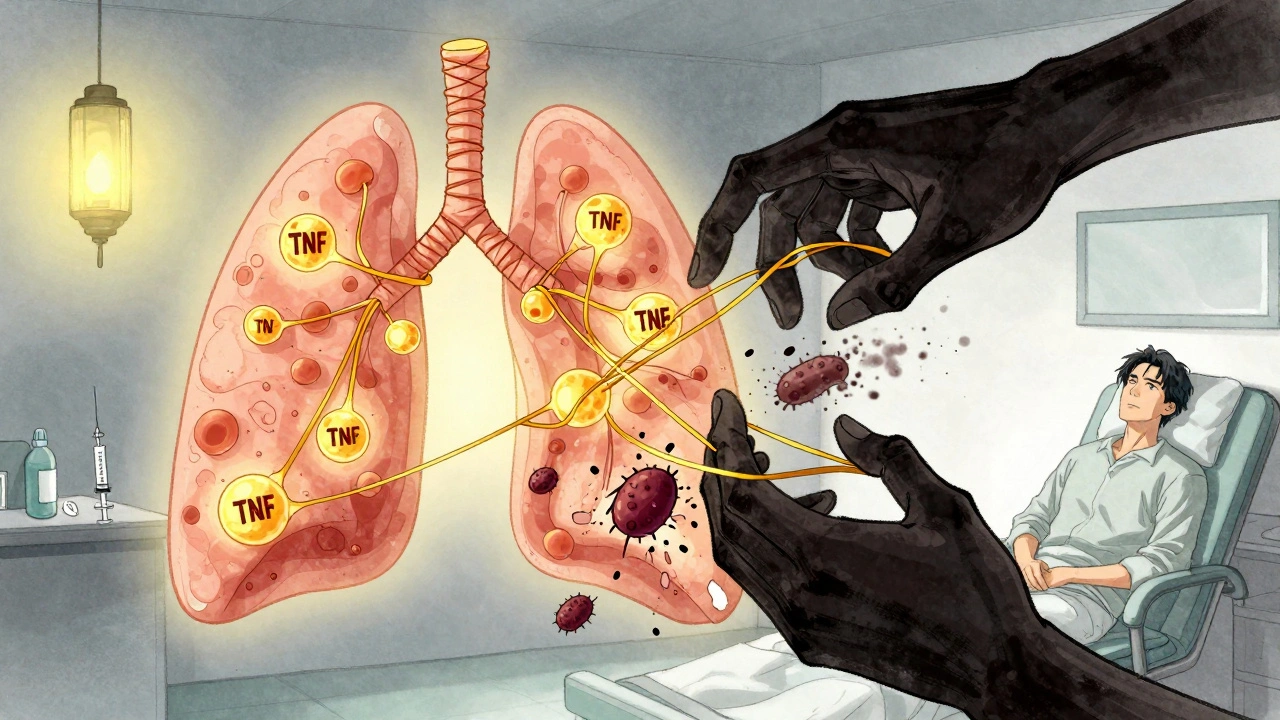
TNF Inhibitors and TB Reactivation: Screening and Monitoring Guidelines
TNF inhibitors effectively treat autoimmune diseases but carry a risk of reactivating latent tuberculosis. Screening with TST or IGRA, treating latent TB before starting therapy, and ongoing symptom monitoring are essential to prevent life-threatening complications.