TNF Inhibitors: What They Are, How They Work, and What You Need to Know
When your immune system turns on your own body, TNF inhibitors, a class of biologic drugs that block tumor necrosis factor, a key driver of inflammation in autoimmune diseases. Also known as anti-TNF agents, these medications help calm down the overactive immune response that causes pain, swelling, and tissue damage in conditions like rheumatoid arthritis, psoriatic arthritis, and Crohn’s disease. They don’t cure these diseases, but for many people, they’re the difference between living with constant pain and getting back to daily life.
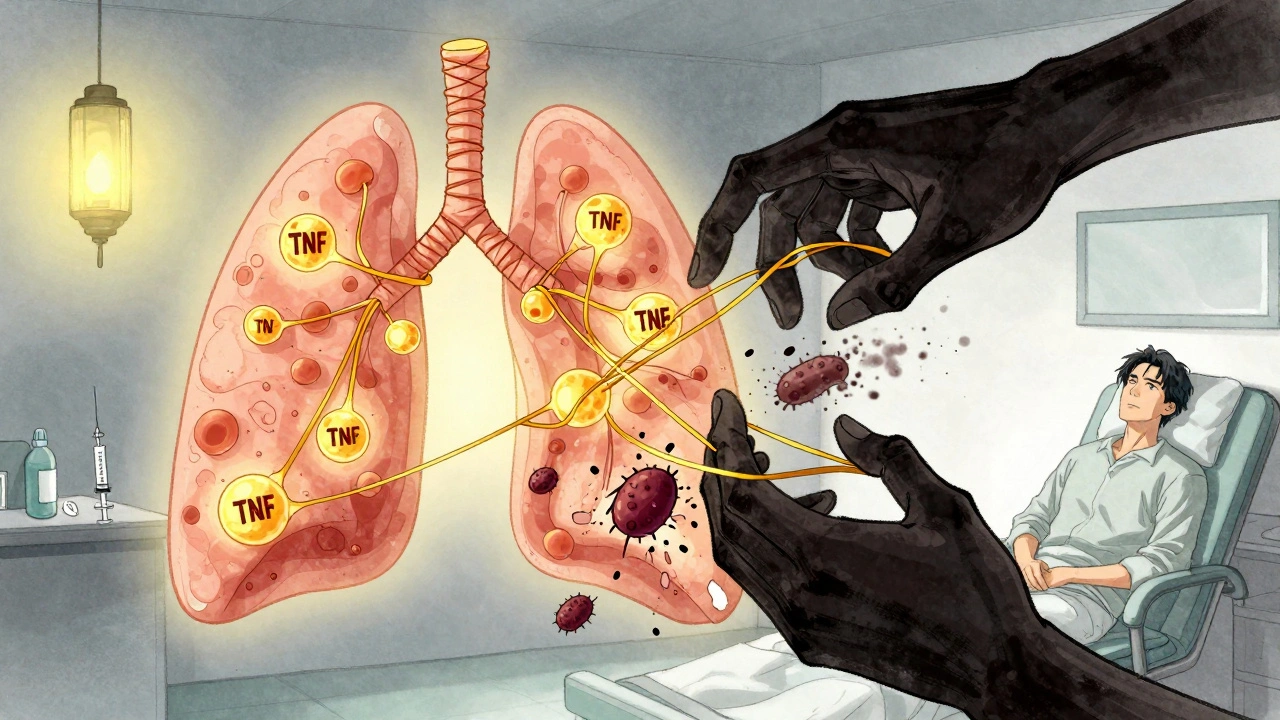
TNF inhibitors work by targeting a specific protein called tumor necrosis factor-alpha, or TNF-alpha. This protein is like a fire alarm in your body—normally it helps fight infection, but in autoimmune diseases, it sounds off constantly, even when there’s no real threat. Drugs like adalimumab, infliximab, and etanercept act like silent alarms, blocking TNF-alpha from triggering inflammation. That’s why they’re so effective for conditions where inflammation is the main problem. But they’re not magic pills. They’re injected or infused, often weekly or monthly, and they come with real risks—like increased chances of serious infections, including tuberculosis. That’s why doctors test for latent TB before starting treatment and monitor patients closely.
These drugs are part of a larger group called biologic drugs, medications made from living cells that target specific parts of the immune system. Unlike older drugs like methotrexate that broadly suppress immunity, biologics are precise. But that precision also means they’re expensive and not for everyone. People with heart failure, multiple sclerosis, or certain cancers often can’t use them. And while they help many with rheumatoid arthritis, a chronic autoimmune disease that attacks the joints, causing pain, stiffness, and deformity, they’re also used for inflammatory bowel disease, a group of conditions including Crohn’s disease and ulcerative colitis that cause gut inflammation. The same drug might be prescribed for both, because the underlying inflammation is similar.
You won’t find TNF inhibitors listed as first-line treatments in most guidelines. They’re usually tried after simpler, cheaper drugs like NSAIDs or DMARDs don’t work well enough. But for those who don’t respond to those, they can be life-changing. Still, they’re not a one-size-fits-all solution. Some people respond quickly. Others need to try several before finding one that works. And some don’t respond at all. That’s why treatment isn’t just about the drug—it’s about matching the right patient to the right therapy, with regular check-ins and smart monitoring.
The posts below cover real-world issues tied to TNF inhibitors and the conditions they treat. You’ll find guides on managing side effects, understanding how these drugs fit into broader treatment plans, and navigating the practical challenges of living with chronic inflammation. Whether you’re a patient, caregiver, or just trying to understand what these drugs really do, this collection gives you the facts without the fluff.
TNF Inhibitors and TB Reactivation: Screening and Monitoring Guidelines
TNF inhibitors effectively treat autoimmune diseases but carry a risk of reactivating latent tuberculosis. Screening with TST or IGRA, treating latent TB before starting therapy, and ongoing symptom monitoring are essential to prevent life-threatening complications.