Type A and Type B Reactions: What They Are and Why They Matter in Medication Safety
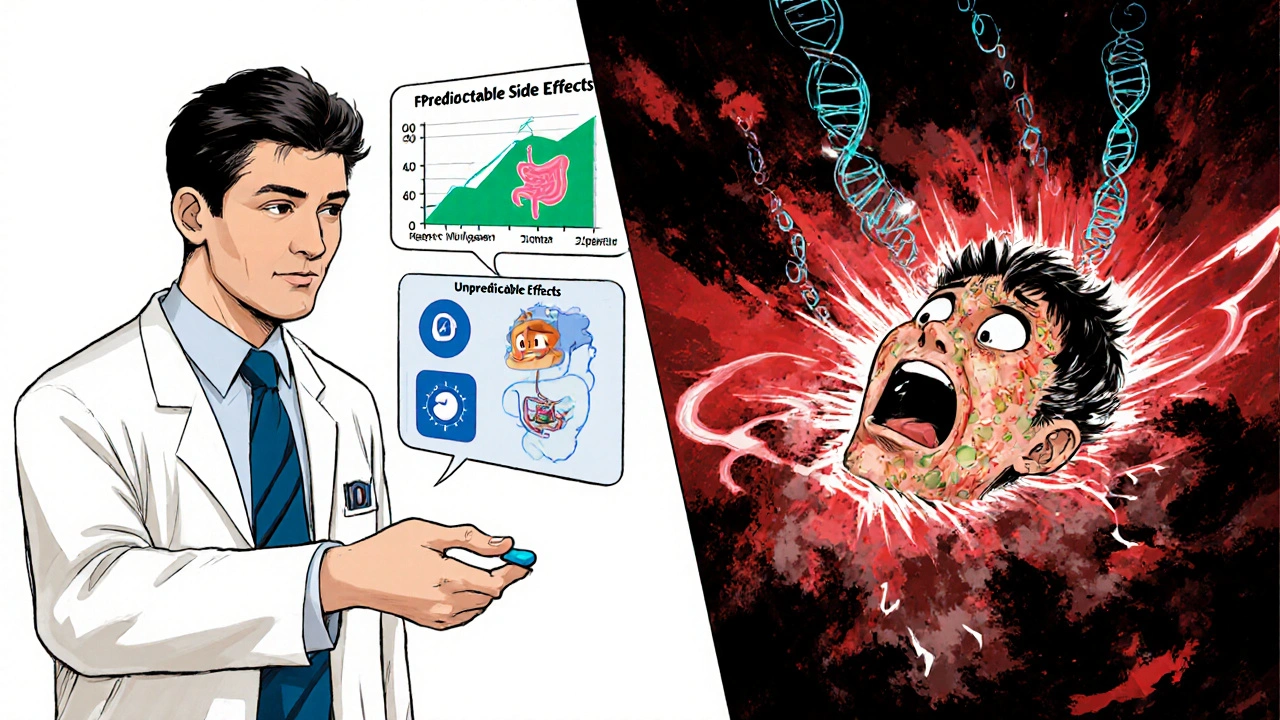
When a drug causes harm, it’s not always because something went wrong—it’s often because of how the drug Type A reactions, predictable, dose-dependent side effects caused by a drug’s known pharmacological action. Also known as augmented reactions, these are the most common kind of adverse drug events you’ll see in clinics and pharmacies. Think of them like too much of a good thing: a blood pressure pill drops your pressure too low, an antibiotic gives you diarrhea because it wipes out good gut bacteria, or a sleep aid leaves you groggy the next day. These aren’t accidents—they’re extensions of the drug’s intended effect, just amplified or mismanaged.
Then there’s Type B reactions, unpredictable, idiosyncratic responses that aren’t tied to the drug’s normal action and often involve the immune system. Also known as bizarre reactions, these are rare but can be life-threatening—like anaphylaxis from penicillin, liver failure from acetaminophen in sensitive people, or Stevens-Johnson syndrome from sulfa drugs. You can’t always test for them beforehand, and they don’t get worse with higher doses. They’re the reason some people react badly to a drug everyone else tolerates fine. Type A reactions make up about 80% of all adverse drug events. Type B reactions are only 10–15%, but they’re the ones that end up in news headlines. Both matter because they shape how doctors choose meds, how pharmacists warn patients, and how you decide whether a side effect is normal or a red flag.
Looking at the posts here, you’ll find real-world examples of both. Antihistamines like Benadryl causing dementia risk? That’s a Type A reaction—long-term anticholinergic burden adds up. MAOIs requiring a tyramine-free diet? That’s Type A too—direct chemical interaction. But if someone breaks out in hives after cold exposure, or has a sudden allergic reaction to a drug they’ve taken for years, that’s Type B. Even something like Cytoxan causing bone marrow suppression? Type A. But if a patient develops a rare autoimmune disorder after chemotherapy? That’s Type B.
Knowing the difference isn’t just for doctors. It helps you ask better questions. Is this side effect something the drug is *supposed* to do, just too much? Or is it something completely unexpected? That changes how you respond. With Type A, you might adjust the dose or switch timing. With Type B, you stop the drug—no exceptions. And that’s why understanding these two categories isn’t just academic—it’s the first step in taking control of your own medication safety.
Predictable vs Unpredictable Side Effects: Understanding Drug Safety
Learn how predictable and unpredictable drug side effects differ, why one is common and manageable while the other is rare but deadly, and what you can do to stay safe on medication.