Warfarin: What It Is, How It Works, and What You Need to Know
When you take warfarin, a prescription blood thinner used to prevent dangerous clots in the heart, legs, or lungs. Also known as Coumadin, it’s one of the most prescribed anticoagulants in the world—used by millions to avoid strokes, pulmonary embolisms, and deep vein thrombosis. Unlike newer drugs, warfarin doesn’t come with a fixed dose. Your body reacts differently, so your doctor has to fine-tune it using regular blood tests.
That’s where INR monitoring, a blood test that measures how long it takes your blood to clot comes in. A normal INR is around 1.0. For most people on warfarin, the target range is 2.0 to 3.0. Too low, and clots can still form. Too high, and you risk bleeding inside your brain, gut, or joints. This isn’t guesswork—it’s science. And it’s why you can’t just take warfarin and forget it. Your diet, other meds, even a cold or flu can throw your INR off track.
Anticoagulant, a class of drugs that slow down the blood’s ability to form clots isn’t just a label—it’s a lifestyle shift. Foods high in vitamin K, like kale, spinach, or broccoli, can make warfarin less effective. Alcohol, certain antibiotics, and even over-the-counter painkillers like ibuprofen can increase bleeding risk. That’s why so many posts on NeoMeds focus on drug interactions, pharmacy delivery for consistent refills, and how to manage chronic meds without missing a day. You’re not just taking a pill—you’re managing a system.
People on warfarin often end up comparing it to newer options like apixaban or rivaroxaban. Those drugs don’t need INR checks, but they’re not always cheaper or covered by insurance. Warfarin still wins on cost—and for many, that matters more than convenience. But it’s also why you’ll find posts here about generic drug savings, how to avoid medication-induced hypertension from other drugs, and why knowing your TE codes (like those from the FDA) helps you swap brands without losing protection.
If you’ve ever had a blood clot, a mechanical heart valve, or atrial fibrillation, warfarin might be part of your daily routine. But it’s not just about the pill. It’s about the lab visits, the food logs, the calls to your pharmacist when you’re sick, and the quiet worry that one missed dose or one extra serving of greens could change everything. The posts below cover exactly that: real stories, practical tips, and hard facts about living with warfarin—whether you’re just starting out or have been on it for years.
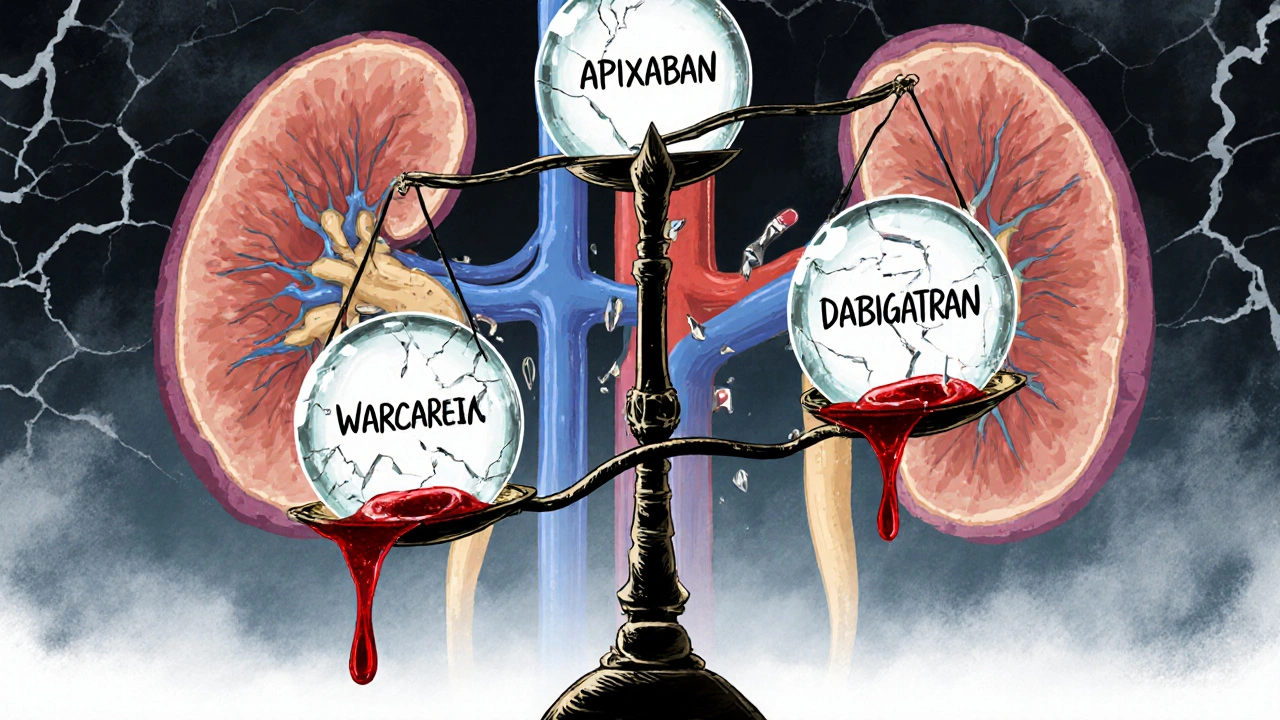
Anticoagulation in Kidney and Liver Disease: What Doctors Really Do
Managing blood thinners in kidney and liver disease is complex. Apixaban is often the safest DOAC, while warfarin remains tricky due to unreliable INR. Real-world data guides decisions when trials don’t.