Prescription Labels: What They Mean and Why They Matter
When you pick up a prescription, the prescription labels, the printed instructions and warnings on medication bottles that guide safe use. Also known as drug labels, they’re your primary tool for avoiding mistakes—yet most people glance at them once and never look again. That’s risky. A single misread dose, missed warning, or misunderstood instruction can lead to hospital visits, dangerous interactions, or even death. The FDA reports that over 1.5 million emergency room visits each year happen because of medication errors, and many start with a misunderstood label.
Behind every prescription label is a system built on science, law, and patient safety. The pharmacy instructions, the specific directions given by the pharmacist on how and when to take the medicine are just one part. You also have drug labeling, the standardized text required by regulators like the FDA that includes dosage, warnings, and active ingredients. Then there’s the medication safety, the practice of using drugs correctly to prevent harm—which depends entirely on whether you understand what’s written on that little paper strip.
Why do people get it wrong? Labels aren’t always clear. Doses like "take twice daily" can mean morning and night—or 12 hours apart. "Take with food" doesn’t say how much food, or what kind. Warnings about alcohol, driving, or other drugs get buried in small print. And if you’re on five meds, reading five different labels, it’s easy to mix them up. That’s why organizing your meds with pill boxes or tracking apps—like the ones covered in our posts—makes a real difference.
You’ll find real-world examples here: how to spot dangerous interactions on a label, what those weird codes like "TE" mean, how to double-check if a generic is truly interchangeable, and why your pharmacist is your best ally when something doesn’t make sense. We cover what to do when a label conflicts with your doctor’s advice, how to read expiration dates correctly, and why storing meds in the bathroom is a bad idea—even if the bottle says "room temperature."
These aren’t theory pages. They’re based on what patients actually face: insulin that loses potency in heat, antihistamines that raise dementia risk, steroids that spike blood sugar, and TB screenings required before starting biologics. Every post ties back to one thing: understanding your prescription label isn’t optional. It’s the first and last line of defense.
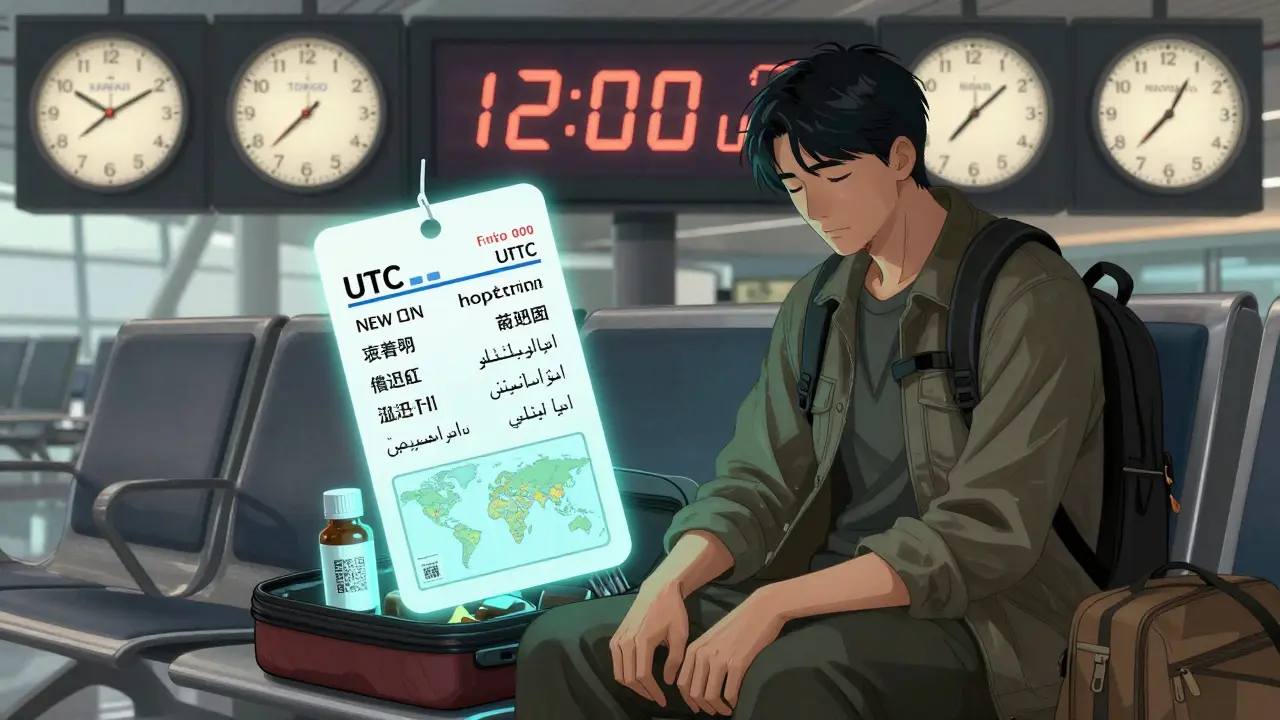
How to Read Prescription Labels When Traveling or Crossing Time Zones
Learn how to read prescription labels for international travel, convert dosing times to UTC, and avoid customs issues or missed doses when crossing time zones. Essential tips for safe, stress-free travel with medication.

Language Barriers and Medication Safety: How to Get Help
Language barriers in healthcare lead to dangerous medication errors. Learn how professional interpreters, translated instructions, and direct observation can prevent harm-and what patients and providers can do to ensure safety.